Chicopee Rehabilitation and Nursing Center
Chicopee Rehabilitation and Nursing Center is a Hospice Home in Massachusetts
Chicopee Rehabilitation and Nursing… is a Hospice Home in Massachusetts
Chicopee Rehabilitation and Nursing Center
Chicopee Rehabilitation and Nursing Center is a Hospice Home in Massachusetts
Chicopee Rehabilitation and Nursing… is a Hospice Home in Massachusetts
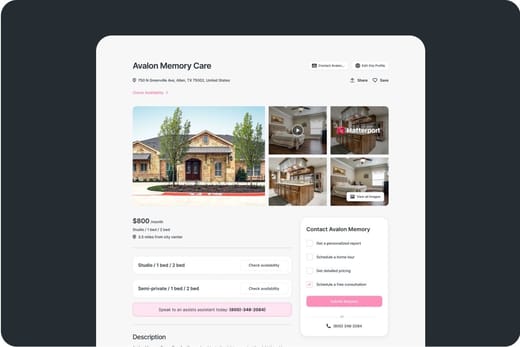
Located in Massachusetts, Chicopee Rehabilitation and Nursing Center has been a pillar of senior care for over 45 years. They provide a range of services, including short-term and long-term care, respite care, IV and antibiotic therapy, hospice care, and more, and they accept various insurances, such as Medicaid, Medicare, and others. Partnering with Mercy Medical Center and Baystate Medical Center, the Chicopee team is experienced in managing various diseases and decreasing symptoms to improve residents’ overall health and well-being.
The center’s clinical capabilities and a wide array of services empower seniors to live their best lives. Beyond medical treatments, they offer activities such as pet therapy and life enhancement to enrich residents’ experiences. Complementary Wi-Fi and satellite TV, as well as outdoor walking paths and garden areas, also help residents stay connected with the outside world.
-
This nursing home maintains occupancy well above most state peers, signaling sustained demand. The property runs a smaller bed inventory than most peers, focusing on a more intimate census. Residents generally stay for shorter periods than state peers, pointing to quicker turnover.
-
Home revenue sits below most peers, indicating modest billing throughput. Payroll costs fall below most facilities, hinting at lean staffing budgets. Total income exceeds the majority of state facilities, highlighting strong profitability.
-
Medicare nights lag behind other facilities, revealing limited Medicare demand. Medicaid nights are roughly in line with the state middle third, maintaining a balanced safety-net share. Private pay nights trail most peers, signaling limited market-rate volume.
 Percentage of home revenue spent on payroll costs.
Percentage of home revenue spent on payroll costs.
 CMS 5-star rating based on health inspections, staffing, and quality measures.
CMS 5-star rating based on health inspections, staffing, and quality measures.
 Rating based on deficiencies found during state health inspections.
Rating based on deficiencies found during state health inspections.
 Rating based on nurse staffing hours per resident per day.
Rating based on nurse staffing hours per resident per day.
 Quality Measures rating based on clinical outcomes for residents.
Quality Measures rating based on clinical outcomes for residents.
 Total nurse staffing hours per resident per day.
Total nurse staffing hours per resident per day.
 Number of resident nights paid by Medicare for short-term or rehab care.
Number of resident nights paid by Medicare for short-term or rehab care.
 Resident nights covered by Medicaid for long-term care or support services.
Resident nights covered by Medicaid for long-term care or support services.
 Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Types of Care at Chicopee Rehabilitation and Nursing Center
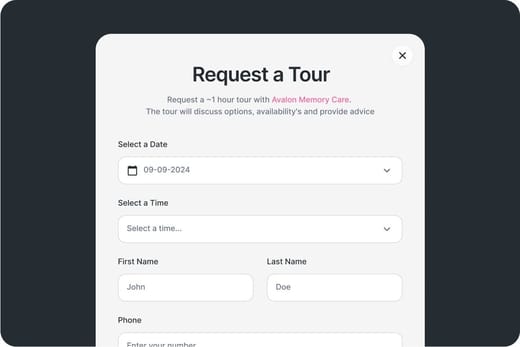
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.
Places of interest near Chicopee Rehabilitation and Nursing Center
6.8 miles from city center
44 New Lombard Rd, Chicopee, MA 01020
Calculate Travel Distance to Chicopee Rehabilitation and Nursing Center
Add your location
Comparison Chart
The information below is reported by the Massachusetts Executive Office of Elder Affairs and Department of Public Health.For seniors needing help with daily tasks but not full-time nursing.
Home Care
Hospice Care
Specialized care for those with Memory Loss, Alzheimer's, or dementia, ensuring safety and support.
Hospice Care
24/7 care needed
Respite Care
Home Care
Hospice Care
Respite Care
Hospice Care
Hospice Care
Staffing Data
Source: CMS Payroll-Based Journal (Q2 2025)
Nursing Staff Breakdown
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 8 | 8.4 | Yes |
| Licensed Practical Nurse | 17 | 8.4 | No |
| Certified Nursing Assistant | 37 | 7.3 | No |
Staff by Category
Contractor Analysis
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 37 | 0 | 37 | 11,365 | 91 | 100% | 7.3 |
| Licensed Practical Nurse | 17 | 0 | 17 | 4,846 | 91 | 100% | 8.4 |
| Occupational Therapy Aide | 18 | 0 | 18 | 4,379 | 91 | 100% | 6 |
| Registered Nurse | 7 | 1 | 8 | 1,415 | 88 | 97% | 8.4 |
| Dietitian | 3 | 0 | 3 | 1,087 | 90 | 99% | 7.5 |
| Respiratory Therapy Technician | 4 | 0 | 4 | 914 | 72 | 79% | 5.9 |
| Physical Therapy Assistant | 4 | 0 | 4 | 528 | 73 | 80% | 6.7 |
| Clinical Nurse Specialist | 1 | 0 | 1 | 480 | 60 | 66% | 8 |
| Administrator | 1 | 0 | 1 | 473 | 63 | 69% | 7.5 |
| Mental Health Service Worker | 2 | 0 | 2 | 421 | 51 | 56% | 7.5 |
| Nurse Practitioner | 1 | 0 | 1 | 416 | 52 | 57% | 8 |
| RN Director of Nursing | 1 | 0 | 1 | 400 | 50 | 55% | 8 |
| Physical Therapy Aide | 2 | 0 | 2 | 327 | 62 | 68% | 5.2 |
| Speech Language Pathologist | 3 | 0 | 3 | 103 | 36 | 40% | 2.9 |
| Qualified Social Worker | 1 | 0 | 1 | 89 | 32 | 35% | 2.8 |
| Occupational Therapy Assistant | 0 | 2 | 2 | 10 | 10 | 11% | 0.9 |
Health Inspection History
Source: CMS Health Citations (Sep 2022 – Feb 2025)
Citation Severity Distribution
Top Deficiency Categories
Citation Sources
State Comparison (MA)
Recent Citations (Last 3 Years)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Feb 18, 2025 | D | Administration | F0849 | Corrected |
| Feb 18, 2025 | D | Environmental | F0908 | Corrected |
| Feb 18, 2025 | D | Infection Control | F0880 | Corrected |
| Feb 18, 2025 | D | Pharmacy | F0756 | Corrected |
| Feb 18, 2025 | D | Quality of Care | F0692 | Corrected |
| Feb 18, 2025 | D | Care Planning | F0637 | Corrected |
| Feb 18, 2025 | B | Care Planning | F0641 | Corrected |
| Feb 18, 2025 | D | Care Planning | F0658 | Corrected |
| Feb 18, 2025 | D | Resident Rights | F0580 | Corrected |
| Feb 28, 2024 | D | Nursing Services | F0710 | Corrected |
| Feb 28, 2024 | F | Nutrition | F0812 | Corrected |
| Feb 28, 2024 | E | Pharmacy | F0761 | Corrected |
| Feb 28, 2024 | E | Quality of Care | F0689 | Corrected |
| Feb 28, 2024 | D | Quality of Care | F0690 | Corrected |
| Feb 28, 2024 | D | Quality of Care | F0693 | Corrected |
| Feb 28, 2024 | D | Quality of Care | F0742 | Corrected |
| Feb 28, 2024 | D | Care Planning | F0656 | Corrected |
| Feb 28, 2024 | C | Resident Rights | F0623 | Corrected |
| Feb 28, 2024 | B | Resident Rights | F0625 | Corrected |
| Sep 28, 2023 | G | Quality of Care | F0689 | Corrected |
| Sep 28, 2023 | G | Care Planning | F0656 | Corrected |
| Sep 14, 2022 | D | Infection Control | F0880 | Corrected |
| Sep 14, 2022 | D | Care Planning | F0656 | Corrected |
| Sep 14, 2022 | D | Care Planning | F0657 | Corrected |
| Sep 14, 2022 | D | Care Planning | F0842 | Corrected |
| Sep 14, 2022 | D | Resident Rights | F0580 | Corrected |
| Sep 14, 2022 | D | Resident Rights | F0584 | Corrected |
Facility Characteristics
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Resident Census by Payment Source
Programs & Services
Family Engagement
Active councils help families stay involved in care decisions and facility operations.
Quality Measures
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Long-Stay Resident Measures
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Short-Stay Resident Measures
Measures for residents who stay 100 days or less (typically rehabilitation patients).
Penalties & Fines
Federal penalties imposed by CMS for regulatory violations, including civil money penalties (fines) and denials of payment for new Medicare/Medicaid admissions.
Source: CMS Penalties Database (Data as of Jan 2026)
Penalty History
Showing all 1 penalties (Sep 2023 - Sep 2023)

Guides for Better Senior Living
From costs to care, explore the most important topics to make informed decisions about your future.
Claim What’s Yours: Financial Aid for Massachusetts Seniors
- General: Age 60+, Massachusetts resident, at risk of nursing home placement.
- Income Limits (2025): ~$1,500/month (individual, varies by region).
- Asset Limits: $2,000 (individual, excludes home, car).
- MA Specifics: Coordinated through Aging Services Access Points (ASAPs); high demand in urban areas.
- Services: In-home care (3-5 hours/day), homemaker services, respite care (up to 14 days/year), adult day care (~$75/day).
- General: Age 65+, Massachusetts resident, Medicaid-eligible, nursing home-level care need.
- Income Limits (2025): ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- MA Specifics: Requires clinical eligibility determination.
- Services: Personal care (5-7 hours/day), respite care (240 hours/year), adult day care (~$75/day), home health services.
- General: Age 65+, Massachusetts resident, eligible for MassHealth (Medicare optional), nursing home-level care need.
- Income Limits (2025): ~$2,829/month (300% FBR, individual); QIT allowed.
- Asset Limits: $2,000 (individual), $3,000 (couple) (excludes home up to $713,000, car).
- MA Specifics: Not available in Dukes/Nantucket Counties; multiple SCO providers (e.g., CCA, Tufts).
- Services: Personal care (5-7 hours/day), medical care, respite (240 hours/year), adult
- General: Age 65+ or disabled, Massachusetts resident, Medicare Part A/B.
- Income Limits (2025): ~$2,510/month (QMB), ~$3,380/month (SLMB), ~$3,598/month (QI)—individual.
- Asset Limits: $9,430 (individual), $14,130 (couple).
- MA Specifics: Three tiers; no waitlist; includes Extra Help for Part D.
- Services: Covers Part B premiums ($174.70/month), deductibles ($240/year), copays (~20%).
- General: Caregivers of 60+ needing care or 55+ caregivers of others; Massachusetts resident; functional needs (2+ ADLs).
- Income Limits (2025): Prioritizes ~$24,980/year (individual); no strict cap.
- Asset Limits: Not assessed; need-based.
- MA Specifics: 27 ASAPs; prioritizes low-income, rural caregivers.
- Services: Respite (4-6 hours/week or 5 days/year), adult day care ($60/day), caregiver training, supplies (~$500/year).
- General: Age 65+ or disabled, Massachusetts resident, enrolled in Medicare Part D (or ineligible for Medicare).
- Income Limits (2025): No strict limit; copays vary by income (~$24,980-$75,000/year individual).
- Asset Limits: Not assessed.
- MA Specifics: Supplements Medicare Part D; no enrollment fee for low-income.
- Services: Covers prescription copays ($5-$40/drug), fills coverage gaps, catastrophic cost protection ($4,000+ covered).
- General: Age 55+, unemployed, low-income, Massachusetts resident.
- Income Limits (2025): ~$1,983/month (125% FPL).
- Asset Limits: Not specified; income-focused.
- MA Specifics: Priority for veterans, rural residents; AARP partnership.
- Services: Paid training (~20 hours/week at ~$15/hour), job placement.
- General: Age 65+ or disabled veteran/spouse, Massachusetts resident, wartime service, need for ADL help (A&A) or homebound.
- Income Limits (2025): Net income < ~$1,984/month (veteran with dependent, A&A); pension offsets income.
- Asset Limits: ~$155,356 (net worth limit).
- MA Specifics: High veteran demand statewide.
- Services: Cash (~$1,433-$2,642/month veteran, ~$951-$1,318 spouse) for care costs (e.g., in-home, assisted living).
Contact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today