Taylor Villa of Mt. San Antonio Gardens
Taylor Villa of Mt. San Antonio Gardens is a Memory Care Home in California
Taylor Villa of Mt.… is a Memory Care Home in California
Taylor Villa of Mt. San Antonio Gardens
Taylor Villa of Mt. San Antonio Gardens is a Memory Care Home in California
Taylor Villa of Mt.… is a Memory Care Home in California
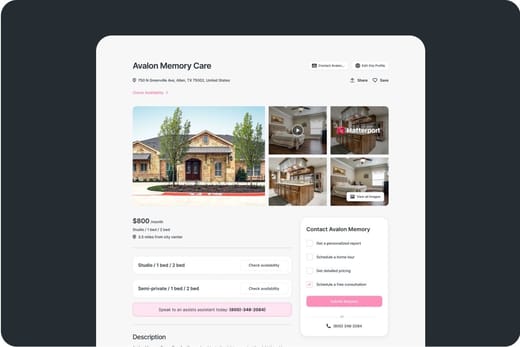
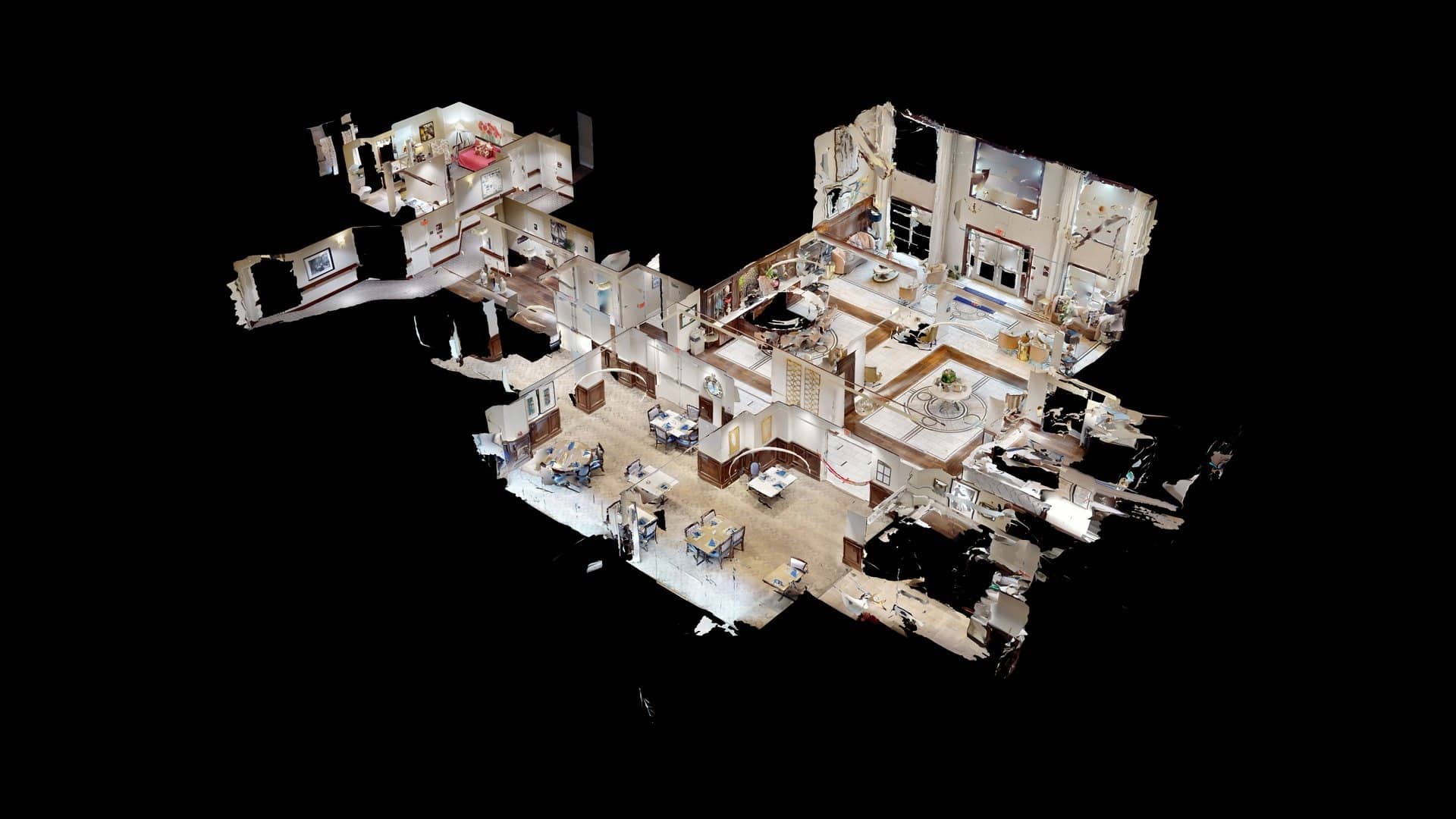
Taylor Villa, located within Mt San Antonio Gardens in Pomona, CA, is a senior living community dedicated to providing quality memory care services to its residents. This senior care home located within the same campus as Harrison Villa and Oak Tree Lodge, is a special unit that provides assisted living services for residents living with Alzheimer’s and other forms of dementia. And as part of those services, they receive round the clock supervision, and life enrichment programs that help the cognitive, creative, physical and psycho-social needs of residents.
As residents of Mt San Antonio Gardens, they also receive the same access to their rich array of amenities. This includes the deliciously prepared meals and snacks, created to cater to the residents’ taste and dietary needs. Their beautifully landscaped courtyard and garden provides relaxing spaces for residents to relax and breathe in fresh air.
-
The facility operates with a larger bed count than most state competitors, supporting broader intake. Residents tend to stay here longer than similar facilities across the state.
-
Home revenue ranks in the upper tier statewide, reflecting strong billing volume. Payroll spending sits in the top tier, showing a strong investment in staffing resources. Total income trails most communities, suggesting tighter operating margins.
-
Medicare nights lag behind other facilities, revealing limited Medicare demand. Medicaid nights fall below most peers, pointing to lighter Medicaid reliance. Private pay nights lead the state, showing strong demand from market-rate residents.
 Percentage of home revenue spent on payroll costs.
Percentage of home revenue spent on payroll costs.
 CMS 5-star rating based on health inspections, staffing, and quality measures.
CMS 5-star rating based on health inspections, staffing, and quality measures.
 Rating based on deficiencies found during state health inspections.
Rating based on deficiencies found during state health inspections.
 Rating based on nurse staffing hours per resident per day.
Rating based on nurse staffing hours per resident per day.
 Quality Measures rating based on clinical outcomes for residents.
Quality Measures rating based on clinical outcomes for residents.
 Total nurse staffing hours per resident per day.
Total nurse staffing hours per resident per day.
 Number of resident nights paid by Medicare for short-term or rehab care.
Number of resident nights paid by Medicare for short-term or rehab care.
 Resident nights covered by Medicaid for long-term care or support services.
Resident nights covered by Medicaid for long-term care or support services.
 Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Nights paid privately by residents or families, without Medicare/Medicaid coverage.
About this community
California average: 71%
Additional licensing details
Ownership & operating entity
Taylor Villa of Mt. San Antonio Gardens is legally operated by CONGREGATIONAL HOMES, INCORPORATED.
Types of Care at Taylor Villa of Mt. San Antonio Gardens
Inspection History
In California, the Department of Social Services (for assisted living facilities) and the Department of Public Health (for nursing homes) conduct inspections to ensure resident safety and regulatory compliance.
12 visits/inspections
3 visits/inspections triggered by complaints
5 other visits
California average: 14 visits/inspections
California average: 12 complaint visits
California average: 3 inspections
Inspection Report Summary for Taylor Villa of Mt. San Antonio Gardens
Mount San Antonio Gardens, a 741‑type continuing‑care retirement community in Pomona, California, was the subject of several unannounced evaluations between 2022 and 2024. The reports highlight the facility’s ongoing compliance with state licensing requirements and its responsiveness to concerns raised by residents, staff, and external stakeholders.
In a required‑one‑year inspection conducted on 9 December 2022, a Licensing Program Analyst reviewed COVID‑19 infection‑control measures. The facility displayed comprehensive signage on hand hygiene, cough etiquette, and PPE use, and staff were observed wearing masks consistently. Vaccination records showed that all residents and staff were fully vaccinated, with only one resident refusing a booster. Food supplies met the agency’s stipulated two‑day perishable and seven‑day non‑perishable thresholds, and the facility’s satellite kitchens and main cafeteria were in good order. Minor technical difficulties were noted during the visit, but no substantive deficiencies were identified.
Three separate complaint investigations followed. The first, filed in November 2021, questioned whether the HomeShip Fund—created to aid residents with monthly fee assistance—was financially secure. After reviewing financial statements and interviewing the executive director, the evaluator found no evidence of insolvency, and the allegation was deemed unsubstantiated. A second investigation in mid‑November 2023 addressed concerns that the facility was retaining a resident requiring higher‑level care and that the resident was not eating properly. Staff and resident interviews, along with file reviews, revealed no corroborating evidence; the allegation was likewise unsubstantiated. The most recent investigation, conducted in June 2024, examined a claim that the dining room environment was unsafe because coffee cup lids did not fit properly. An on‑site tour and resident interviews confirmed that cups were sealed correctly and that residents reported feeling safe, leading to an unsubstantiated outcome.
Across all reviews, the facility consistently demonstrates adherence to licensing standards, maintains adequate infection‑control and food‑service protocols, and shows a pattern of addressing complaints through thorough documentation and staff engagement. While a number of allegations were lodged, none were substantiated, suggesting either low risk of regulatory violations or that the complaints lacked sufficient evidence. Overall, Mount San Antonio Gardens appears to provide a safe, compliant environment for its residents.
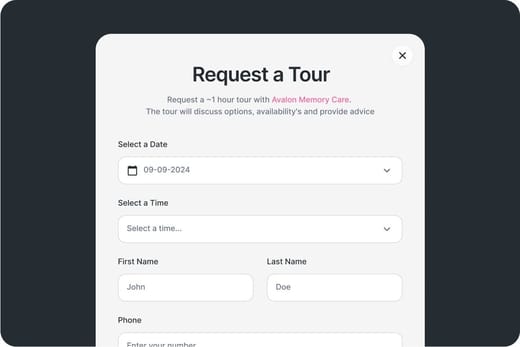
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.
Places of interest near Taylor Villa of Mt. San Antonio Gardens
3.7 miles from city center
900 Harrison Ave, Pomona, CA 91767
Calculate Travel Distance to Taylor Villa of Mt. San Antonio Gardens
Add your location
Staffing Data
Source: CMS Payroll-Based Journal (Q2 2025)
Nursing Staff Breakdown
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 9 | 7.8 | No |
| Licensed Practical Nurse | 16 | 7.5 | No |
| Certified Nursing Assistant | 35 | 7.5 | No |
Staff by Category
Contractor Analysis
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 35 | 0 | 35 | 13,406 | 91 | 100% | 7.5 |
| Licensed Practical Nurse | 16 | 0 | 16 | 4,607 | 91 | 100% | 7.5 |
| Registered Nurse | 9 | 0 | 9 | 2,168 | 89 | 98% | 7.8 |
| RN Director of Nursing | 2 | 0 | 2 | 952 | 62 | 68% | 8 |
| Other Dietary Services Staff | 5 | 0 | 5 | 642 | 77 | 85% | 7.4 |
| Occupational Therapy Aide | 0 | 2 | 2 | 512 | 64 | 70% | 8 |
| Respiratory Therapy Technician | 0 | 7 | 7 | 509 | 71 | 78% | 4.5 |
| Administrator | 1 | 0 | 1 | 504 | 63 | 69% | 8 |
| Nurse Practitioner | 1 | 0 | 1 | 504 | 63 | 69% | 8 |
| Mental Health Service Worker | 1 | 0 | 1 | 488 | 61 | 67% | 8 |
| Speech Language Pathologist | 0 | 3 | 3 | 285 | 60 | 66% | 3.1 |
| Physical Therapy Aide | 0 | 6 | 6 | 284 | 65 | 71% | 4.2 |
| Physical Therapy Assistant | 0 | 3 | 3 | 244 | 61 | 67% | 3.9 |
| Medical Director | 0 | 1 | 1 | 30 | 18 | 20% | 1.7 |
| Qualified Social Worker | 0 | 3 | 3 | 30 | 16 | 18% | 1.9 |
| Other Physician | 0 | 1 | 1 | 18 | 9 | 10% | 2 |
Health Inspection History
Source: CMS Health Citations (May 2023 – May 2025)
Citation Severity Distribution
Top Deficiency Categories
Citation Sources
State Comparison (CA)
Recent Citations (Last 3 Years)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| May 30, 2025 | D | Quality of Care | F0684 | Corrected |
| May 30, 2025 | D | Quality of Care | F0690 | Corrected |
| May 30, 2025 | D | Quality of Care | F0700 | Corrected |
| May 30, 2025 | D | Care Planning | F0842 | Corrected |
| May 16, 2024 | D | Infection Control | F0880 | Corrected |
| May 16, 2024 | E | Nutrition | F0812 | Corrected |
| May 16, 2024 | D | Quality of Care | F0684 | Corrected |
| May 16, 2024 | D | Care Planning | F0641 | Corrected |
| May 26, 2023 | E | Infection Control | F0880 | Corrected |
| May 26, 2023 | D | Nutrition | F0805 | Corrected |
| May 26, 2023 | D | Pharmacy | F0759 | Corrected |
| May 26, 2023 | D | Quality of Care | F0686 | Corrected |
| May 26, 2023 | E | Quality of Care | F0688 | Corrected |
| May 26, 2023 | D | Quality of Care | F0695 | Corrected |
| May 26, 2023 | D | Resident Rights | F0550 | Corrected |
| May 26, 2023 | D | Resident Rights | F0558 | Corrected |
Facility Characteristics
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Resident Census by Payment Source
Programs & Services
Family Engagement
Active councils help families stay involved in care decisions and facility operations.
Quality Measures
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Long-Stay Resident Measures
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Short-Stay Resident Measures
Measures for residents who stay 100 days or less (typically rehabilitation patients).

Guides for Better Senior Living
From costs to care, explore the most important topics to make informed decisions about your future.
Claim What’s Yours: Financial Aid for California Seniors
- General: Age 65+, California resident, Medi-Cal eligible, nursing home risk.
- Income Limits (2025): ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- CA Specifics: County-managed; waitlists possible.
- Services: In-home support (4-6 hours/day), respite care (14 days/year), meals (~$6/meal), transportation (8 trips/month), care management.
- General: Age 65+, California resident, Medicaid-eligible or low-income.
- Income Limits: ~$1,732/month (individual, Medi-Cal threshold).
- Asset Limits: $2,000 (individual).
- CA Specifics: Can hire family as caregivers.
- Services: Personal care (up to 283 hours/month), homemaker services, respite (varies).
- General: Age 65+, California resident, Medi-Cal-eligible, nursing home-eligible but community-capable.
- Income Limits: ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual).
- CA Specifics: Available in 38 counties; waitlists common.
- Services: Case management, respite care (up to 10 days/year), minor home mods (avg. $500), adult day care (~$50/day).
- General: Age 62+, California resident, own and live in home, 40% equity.
- Income Limits (2025): ~$51,500/year (household, adjusted annually).
- Asset Limits: Equity-based; no strict asset cap.
- CA Specifics: Deferred taxes accrue interest (5% as of 2024); repaid upon sale/death.
- Services: Property tax deferral (avg. $1,000-$3,000/year, varies by county).
- General: Age 65+ or disabled, California resident, Medi-Cal-eligible, nursing home-eligible.
- Income Limits: ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual).
- CA Specifics: Available in 15 counties (e.g., LA, Sacramento); waitlists common.
- Services: Personal care in ALFs (5-7 hours/day), medication management, social services.
- General: Caregivers of California residents 60+ needing help with 3+ daily activities; no caregiver age limit.
- Income Limits: No strict limit; cost-sharing above ~$2,500/month threshold.
- Asset Limits: Not applicable; need-based.
- CA Specifics: High demand in urban areas; complements IHSS respite.
- Services: Respite care (up to 10 days/year), counseling (4-6 sessions/year), training (2-3 workshops/year), supplies (~$200/year).
- General: Age 60+ priority, California resident, low-income, utility/heating need.
- Income Limits (2025): ~$2,510/month (200% of poverty level, individual).
- Asset Limits: Not applicable; income-focused.
- CA Specifics: High demand in inland/coastal extremes; weatherization capped at $5,000/home.
- Services: Utility payments (avg. $500-$1,000/year), weatherization (e.g., insulation, avg. $1,000-$3,000 savings).
Contact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today