Maple Springs of North Logan
Maple Springs of North Logan is an Assisted Living Home in Utah
Maple Springs of North… is an Assisted Living Home in Utah
Maple Springs of North Logan
Maple Springs of North Logan is an Assisted Living Home in Utah
Maple Springs of North… is an Assisted Living Home in Utah
Tucked in the tranquil neighborhood of North Logan, UT, Maple Springs of North Logan is dedicated to improving seniors’ well-being with assisted living, memory care, skilled nursing, and rehabilitation services. Seniors and families can keep their peace of mind with a team of responsive and highly trained professionals caring for their needs and aspirations 24/7. Moreover, the community promotes a bright and welcoming environment for seniors to flourish and live their lives to the fullest.
Residents do not run out of things to do with a lot of enriching activities and engaging programs that aim to keep them happy and socially connected. Here, delectable and healthy meals are served to satisfy nutritional needs and tastes. Amenities include a movie theater, onsite salon services, a library, and an ice cream parlor.
-
Occupancy trails most facilities in the state, suggesting excess open capacity. Bed capacity aligns with the typical community size in the state, allowing steady admissions. Residents generally stay for shorter periods than state peers, pointing to quicker turnover.
-
Home revenue lands near the state median, signaling steady but not standout inflows. Payroll spending sits in the top tier, showing a strong investment in staffing resources. Total income trails most communities, suggesting tighter operating margins.
-
Medicare nights lag behind other facilities, revealing limited Medicare demand. Medicaid nights sit above most state facilities, underscoring deep Title XIX coverage. Private pay nights lead the state, showing strong demand from market-rate residents.
 Percentage of home revenue spent on payroll costs.
Percentage of home revenue spent on payroll costs.
 CMS 5-star rating based on health inspections, staffing, and quality measures.
CMS 5-star rating based on health inspections, staffing, and quality measures.
 Rating based on deficiencies found during state health inspections.
Rating based on deficiencies found during state health inspections.
 Rating based on nurse staffing hours per resident per day.
Rating based on nurse staffing hours per resident per day.
 Quality Measures rating based on clinical outcomes for residents.
Quality Measures rating based on clinical outcomes for residents.
 Total nurse staffing hours per resident per day.
Total nurse staffing hours per resident per day.
 Number of resident nights paid by Medicare for short-term or rehab care.
Number of resident nights paid by Medicare for short-term or rehab care.
 Resident nights covered by Medicaid for long-term care or support services.
Resident nights covered by Medicaid for long-term care or support services.
 Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Nights paid privately by residents or families, without Medicare/Medicaid coverage.
About this community
Additional licensing details
What does this home offer?
Total Residents: 100 Residents
Housing Options: Studio
Building Type: 2-story
Total Residents
Transportation Services
Fitness and Recreation
Types of Care at Maple Springs of North Logan
Inspection History
In Utah, the Department of Health and Human Services, Health Facility Licensing conducts regular onsite inspections to ensure compliance with state and federal healthcare standards.
5 visits/inspections
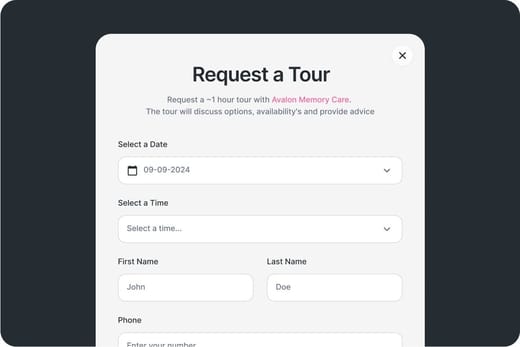
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.
Places of interest near Maple Springs of North Logan
1.2 miles from city center
350 E 2200 N, North Logan, UT 84341
Calculate Travel Distance to Maple Springs of North Logan
Add your location
Staffing Data
Source: CMS Payroll-Based Journal (Q2 2025)
Nursing Staff Breakdown
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 18 | 9.6 | No |
| Licensed Practical Nurse | 13 | 9 | No |
| Certified Nursing Assistant | 61 | 6.3 | No |
Staff by Category
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 61 | 0 | 61 | 12,123 | 91 | 100% | 6.3 |
| Registered Nurse | 18 | 0 | 18 | 4,093 | 91 | 100% | 9.6 |
| Licensed Practical Nurse | 13 | 0 | 13 | 3,161 | 91 | 100% | 9 |
| Physical Therapy Assistant | 2 | 0 | 2 | 896 | 81 | 89% | 6.4 |
| Respiratory Therapy Technician | 4 | 0 | 4 | 792 | 73 | 80% | 7.1 |
| Administrator | 1 | 0 | 1 | 480 | 64 | 70% | 7.5 |
| Nurse Practitioner | 1 | 0 | 1 | 450 | 60 | 66% | 7.5 |
| Dietitian | 1 | 0 | 1 | 439 | 52 | 57% | 8.4 |
| Physical Therapy Aide | 1 | 0 | 1 | 400 | 63 | 69% | 6.4 |
| Other Dietary Services Staff | 1 | 0 | 1 | 353 | 39 | 43% | 9 |
| Speech Language Pathologist | 2 | 0 | 2 | 301 | 52 | 57% | 4.6 |
| Medical Director | 1 | 0 | 1 | 260 | 65 | 71% | 4 |
| Clinical Nurse Specialist | 1 | 0 | 1 | 260 | 65 | 71% | 4 |
| Feeding Assistant | 1 | 0 | 1 | 260 | 65 | 71% | 4 |
| Dental Services Staff | 1 | 0 | 1 | 196 | 27 | 30% | 7.2 |
| Occupational Therapy Aide | 1 | 0 | 1 | 85 | 13 | 14% | 6.5 |
| Qualified Social Worker | 1 | 0 | 1 | 52 | 31 | 34% | 1.7 |
Health Inspection History
Source: CMS Health Citations (Sep 2019 – Nov 2023)
Citation Severity Distribution
Top Deficiency Categories
Citation Sources
State Comparison (UT)
Recent Citations (Last 3 Years)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Nov 16, 2023 | D | Abuse/Neglect | F0609 | Corrected |
| Nov 16, 2023 | D | Administration | F0770 | Corrected |
| Nov 16, 2023 | D | Administration | F0775 | Corrected |
| Nov 16, 2023 | D | Infection Control | F0881 | Corrected |
| Nov 16, 2023 | E | Nutrition | F0812 | Corrected |
| Nov 16, 2023 | D | Pharmacy | F0757 | Corrected |
| Nov 16, 2023 | D | Pharmacy | F0758 | Corrected |
| Nov 16, 2023 | D | Quality of Care | F0686 | Corrected |
| Nov 16, 2023 | D | Quality of Care | F0689 | Corrected |
| Nov 16, 2023 | D | Care Planning | F0842 | Corrected |
| Nov 16, 2023 | D | Resident Rights | F0580 | Corrected |
| Nov 16, 2023 | E | Resident Rights | F0622 | Corrected |
| Jan 13, 2022 | F | Infection Control | F0880 | Corrected |
| Jan 13, 2022 | E | Infection Control | F0886 | Corrected |
| Jan 13, 2022 | D | Nursing Services | F0712 | Corrected |
| Jan 13, 2022 | E | Care Planning | F0842 | Corrected |
| Sep 26, 2019 | D | Administration | F0770 | Corrected |
| Sep 26, 2019 | E | Infection Control | F0880 | Corrected |
| Sep 26, 2019 | E | Infection Control | F0881 | Corrected |
| Sep 26, 2019 | D | Infection Control | F0883 | Corrected |
| Sep 26, 2019 | D | Nursing Services | F0712 | Corrected |
| Sep 26, 2019 | D | Nutrition | F0806 | Corrected |
| Sep 26, 2019 | E | Nutrition | F0812 | Corrected |
| Sep 26, 2019 | D | Pharmacy | F0757 | Corrected |
| Sep 26, 2019 | D | Pharmacy | F0758 | Corrected |
| Sep 26, 2019 | E | Pharmacy | F0759 | Corrected |
| Sep 26, 2019 | D | Pharmacy | F0760 | Corrected |
| Sep 26, 2019 | D | Pharmacy | F0761 | Corrected |
| Sep 26, 2019 | D | Quality of Care | F0676 | Corrected |
| Sep 26, 2019 | E | Quality of Care | F0684 | Corrected |
| Sep 26, 2019 | E | Resident Rights | F0550 | Corrected |
| Sep 26, 2019 | D | Resident Rights | F0580 | Corrected |
Facility Characteristics
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Resident Census by Payment Source
Programs & Services
Family Engagement
Active councils help families stay involved in care decisions and facility operations.
Quality Measures
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Long-Stay Resident Measures
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Short-Stay Resident Measures
Measures for residents who stay 100 days or less (typically rehabilitation patients).

Guides for Better Senior Living
From costs to care, explore the most important topics to make informed decisions about your future.
Claim What’s Yours: Financial Aid for Utah Seniors
- General: Age 65+, Utah resident, Medicaid-eligible, nursing home-level care need.
- Income Limits (2025): ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- UT Specifics: Rural challenges; waitlists possible.
- Services: Personal care (5-7 hours/day), respite (240 hours/year), adult day care ($65/day), home modifications ($1,500 avg.).
- General: Age 60+, Utah resident, at risk of nursing home.
- Income Limits: ~$2,000/month (individual, varies).
- Asset Limits: $5,000 (individual).
- UT Specifics: Limited funding; rural focus.
- Services: In-home care (3-5 hours/week), respite (up to 10 days/year), transportation (~5 trips/month).
- General: Age 60+, UT resident; no income/asset limits.
- Income Limits (2025): None; donations encouraged.
- Asset Limits: Not assessed.
- UT Specifics: 12 AAAs; includes Meals on Wheels; rural emphasis.
- Services: Meals (~$5-$7/meal), transportation, homemaker services (~4 hours/week), respite (5 days/year), legal aid.
- General: Age 65+ or disabled, UT resident, Medicare Part A/B.
- Income Limits (2025): ~$2,510/month (QMB), ~$3,380/month (SLMB), ~$3,598/month (QI)—individual.
- Asset Limits: $9,430 (individual), $14,130 (couple).
- UT Specifics: Includes Extra Help for Part D; no waitlist.
- Services: Covers Part B premiums ($174.70/month), deductibles ($240/year), copays (~20%).
- General: Age 60+ prioritized, UT resident, low-income household.
- Income Limits (2025): ~$3,970/month (185% FPL).
- Asset Limits: Not assessed.
- UT Specifics: Covers gas, electric, propane; emergency aid available.
- Services: Heating/cooling aid ($300-$1,000/season), crisis aid ($500 max).
- General: Caregivers of 60+ needing care or 55+ caregivers of others; UT resident; 2+ ADLs.
- Income Limits (2025): No strict cap; prioritizes low-income (~$24,980/year).
- Asset Limits: Not assessed.
- UT Specifics: Includes grandparent caregivers; serves ~1,500 annually.
- Services: Respite (4-6 hours/week or 5 days/year), adult day care ($60/day), training, supplies (~$500/year).
- General: Age 55+, unemployed, low-income, UT resident.
- Income Limits (2025): ~$1,983/month (125% FPL).
- Asset Limits: Not specified.
- UT Specifics: Priority for veterans, rural residents; AARP partnership.
- Services: Paid training (~20 hours/week at ~$7.25/hour), job placement.
- General: Age 65+ or disabled veteran/spouse, UT resident, wartime service, ADL help (A&A) or homebound.
- Income Limits (2025): Net income < ~$1,984/month (veteran with dependent, A&A); pension offsets income.
- Asset Limits: ~$155,356 (net worth).
- UT Specifics: Supports rural veterans; high demand near VA centers.
- Services: Cash (~$1,433-$2,642/month veteran, ~$951-$1,318 spouse) for care costs.
- General: Age 66+ (abatement) or 75+ (deferral), UT resident 10+ months/year, homeowner.
- Income Limits (2025): ~$40,000/year (household, abatement); no limit for deferral.
- Asset Limits: Not assessed; home value < ~$500,000 typical.
- UT Specifics: Abatement up to $1,200; deferral accrues interest (2.5%-5%).
- Services: Tax relief (~$500-$1,200/year) or deferral (postpones payment).
- General: Age 60+, UT resident, low-income.
- Income Limits (2025): ~$2,322/month (185% FPL).
- Asset Limits: Not assessed.
- UT Specifics: Vouchers (~$50/season); serves ~5,000 via 12 AAAs.
- Services: Vouchers (~$50/season) for produce at farmers’ markets.
Contact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today