Green Hills Center for Rehabilitation
Green Hills Center for Rehabilitation
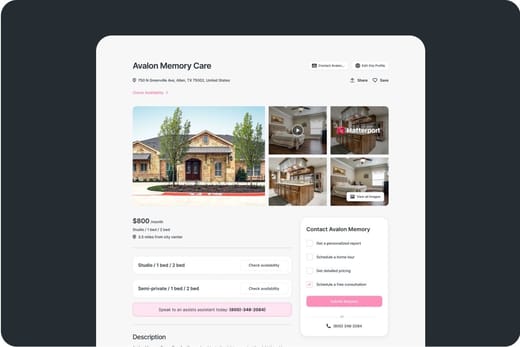
Green Hills Center for Rehabilitation is a community that proudly elevates the recovery experience of its residents. A premier nursing home that has been awarded a list of accolades, some of which are from the U.S. News and World Report ranking them as the Best Nursing Home; they have exceeded expectations for its short-term care. Green Hills Center for Rehabilitation is a tightly-knit community where residents are able to relax and renew themselves.
A member of the CareRite healthcare, Green Hills offers an array of recovery services that help a fast healing journey– orthopedic rehabilitation, short-term and long-term rehabilitation, amputee care, and wound care. Other luxurious services include its chef-prepared meals in a restaurant-style dining service.
Mackenzie Cannon serves as the Administrator at Green Hills Center for Rehabilitation. She leads a dedicated team focused on compassionate care, ensuring patients’ well-being through kindness, professionalism, and a supportive environment that promotes healing both physically and emotionally.
Compare Nursing Homes around Nashville
The information below is reported by the Tennessee Department of Health, Division of Health Care Facilities.Nursing Home 24/7 care needed
Assisted Living For seniors needing help with daily tasks but not full-time nursing.
Nursing Home 24/7 care needed
Assisted Living For seniors needing help with daily tasks but not full-time nursing.
Nursing Home 24/7 care needed
Assisted Living For seniors needing help with daily tasks but not full-time nursing.
Nursing Home 24/7 care needed
Assisted Living For seniors needing help with daily tasks but not full-time nursing.
Nursing Home 24/7 care needed
Assisted Living For seniors needing help with daily tasks but not full-time nursing.
Guides for Better Senior Living
Care Cost Calculator: See Prices in Your Area
Nursing Home Data Explorer
Don’t Wait Too Long: 7 Red Flag Signs Your Parent Needs Assisted Living Now
The True Cost of Assisted Living in 2025 – And How Families Are Paying For It
Understanding Senior Living Costs: Pricing Models, Discounts & Financial Assistance
Financial Aid for Tennessee Seniors
Get financial aid guidanceContact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today
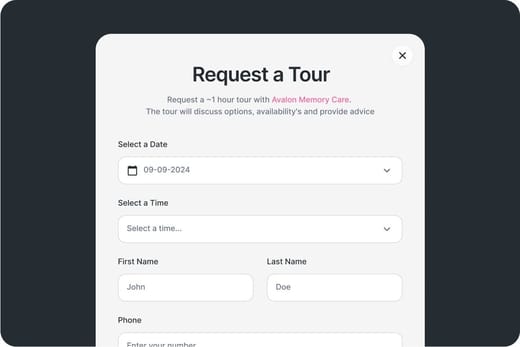
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.