Primarily short stays
Residents typically stay for brief periods, with frequent admissions and discharges throughout the year.
We arrange tours, appointments, and even moving support so you don’t have to
May offer a more intimate, personalized care environment.
Lower occupancy suggests more openings may be available.
Residents typically stay for brief periods, with frequent admissions and discharges throughout the year.
22% of new residents, usually for short-term rehab.
74% of new residents, often for short stays.
4% of new residents, often for long-term daily care.
 The portion of the home's budget spent on staff, including nurses, caregivers, and other employees who support care and operations.
The portion of the home's budget spent on staff, including nurses, caregivers, and other employees who support care and operations.
 All remaining costs needed to run the home, such as food, utilities, building maintenance, supplies and administrative expenses.
All remaining costs needed to run the home, such as food, utilities, building maintenance, supplies and administrative expenses.
Indigo Manor Nursing & Rehabilitation is legally operated by BEDROCK HCS AT DAYTONA FL LLC, and administrated by KENNETH D NICHOLS.
In Florida, the Agency for Health Care Administration (AHCA) is the primary authority that conducts unannounced inspections and completes official health quality reports for all healthcare facilities.
7 with citations
11 without citations
Florida average: 17 inspections with citations
Citations indicate regulatory violations. A higher number implies the facility had several areas requiring improvement.
Florida average: 34 citations
Penalties or interventions imposed by state regulators when facilities do not comply with quality, safety or regulatory standards.
10/6/2022: Survey
Florida average: 5 enforcement actions
INDIGO PALMS AT THE MANOR was inspected on 2025-04-15, with deficiencies cited. During the reporting period from 2012-11-20 to 2025-04-15, a total of 18 inspections were conducted, all of which resulted in deficiencies being identified. The facility accumulated a total of 30 line-item deficiencies across these inspections, which included standard, complaint, and monitor types. Key themes emerged in the inspection reports, focusing on records/documentation and resident care/rights. While no evidence indicates that all cited deficiencies have been corrected, the facility's latest status reflects ongoing efforts to address these issues.
5.1 miles from city center
595 N Williamson Blvd, Daytona Beach, FL 32114
Add your location
Source: CMS Payroll-Based Journal (Q2 2025)
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 21 | 8.7 | No |
| Licensed Practical Nurse | 32 | 9.6 | No |
| Certified Nursing Assistant | 87 | 7.9 | No |
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 87 | 0 | 87 | 26,908 | 91 | 100% | 7.9 |
| Licensed Practical Nurse | 32 | 0 | 32 | 9,391 | 91 | 100% | 9.6 |
| Registered Nurse | 21 | 0 | 21 | 4,639 | 91 | 100% | 8.7 |
| Speech Language Pathologist | 8 | 0 | 8 | 1,897 | 88 | 97% | 7 |
| Clinical Nurse Specialist | 5 | 0 | 5 | 1,565 | 82 | 90% | 7.2 |
| Physical Therapy Aide | 5 | 0 | 5 | 1,362 | 89 | 98% | 7.7 |
| Administrator | 2 | 0 | 2 | 1,024 | 64 | 70% | 8 |
| RN Director of Nursing | 4 | 0 | 4 | 871 | 86 | 95% | 5.1 |
| Other Dietary Services Staff | 2 | 0 | 2 | 826 | 81 | 89% | 7.7 |
| Feeding Assistant | 0 | 3 | 3 | 648 | 89 | 98% | 4.9 |
| Respiratory Therapy Technician | 3 | 0 | 3 | 558 | 83 | 91% | 6.5 |
| Dietitian | 1 | 0 | 1 | 512 | 64 | 70% | 8 |
| Mental Health Service Worker | 1 | 0 | 1 | 512 | 64 | 70% | 8 |
| Physical Therapy Assistant | 3 | 0 | 3 | 505 | 78 | 86% | 6.5 |
| Qualified Social Worker | 2 | 0 | 2 | 499 | 65 | 71% | 7.7 |
| Nurse Practitioner | 1 | 0 | 1 | 488 | 61 | 67% | 8 |
| Dental Services Staff | 2 | 0 | 2 | 371 | 52 | 57% | 7.1 |
| Occupational Therapy Aide | 1 | 0 | 1 | 320 | 44 | 48% | 7.3 |
| Other Physician | 0 | 2 | 2 | 232 | 64 | 70% | 3 |
| Occupational Therapy Assistant | 0 | 1 | 1 | 49 | 8 | 9% | 6.1 |
| Medical Director | 0 | 1 | 1 | 36 | 18 | 20% | 2 |
Source: CMS Health Citations (Jul 2021 – Mar 2025)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Mar 13, 2025 | F | Nutrition | F0812 | Corrected |
| Mar 13, 2025 | D | Pharmacy | F0759 | Corrected |
| Mar 13, 2025 | D | Quality of Care | F0677 | Corrected |
| Mar 13, 2025 | D | Quality of Care | F0689 | Corrected |
| Mar 13, 2025 | D | Quality of Care | F0695 | Corrected |
| Oct 03, 2023 | F | Environmental | F0921 | Corrected |
| Oct 03, 2023 | E | Resident Rights | F0569 | Corrected |
| Apr 13, 2023 | J | Abuse/Neglect | F0600 | Corrected |
| Apr 13, 2023 | E | Infection Control | F0880 | Corrected |
| Apr 13, 2023 | F | Nutrition | F0812 | Corrected |
| Apr 13, 2023 | D | Pharmacy | F0755 | Corrected |
| Apr 13, 2023 | D | Pharmacy | F0757 | Corrected |
| Apr 13, 2023 | D | Pharmacy | F0759 | Corrected |
| Apr 13, 2023 | E | Pharmacy | F0761 | Corrected |
| Apr 13, 2023 | D | Quality of Care | F0689 | Corrected |
| Apr 13, 2023 | D | Quality of Care | F0695 | Corrected |
| Apr 13, 2023 | D | Quality of Care | F0698 | Corrected |
| Apr 13, 2023 | D | Care Planning | F0644 | Corrected |
| Apr 13, 2023 | D | Care Planning | F0842 | Corrected |
| Apr 13, 2023 | D | Resident Rights | F0582 | Corrected |
| Apr 13, 2023 | D | Resident Rights | F0583 | Corrected |
| Jul 09, 2021 | F | Nutrition | F0812 | Corrected |
| Jul 09, 2021 | D | Pharmacy | F0761 | Corrected |
| Jul 09, 2021 | D | Quality of Care | F0690 | Corrected |
| Jul 09, 2021 | D | Quality of Care | F0697 | Corrected |
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Active councils help families stay involved in care decisions and facility operations.
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Measures for residents who stay 100 days or less (typically rehabilitation patients).
Federal penalties imposed by CMS for regulatory violations, including civil money penalties (fines) and denials of payment for new Medicare/Medicaid admissions.
Source: CMS Penalties Database (Data as of Jan 2026)
Showing all 5 penalties (Apr 2023 - Mar 2025)
Historical financial and operational data for Indigo Manor Nursing & Rehabilitation based on CMS SNF Cost Reports.
Loading trend charts...
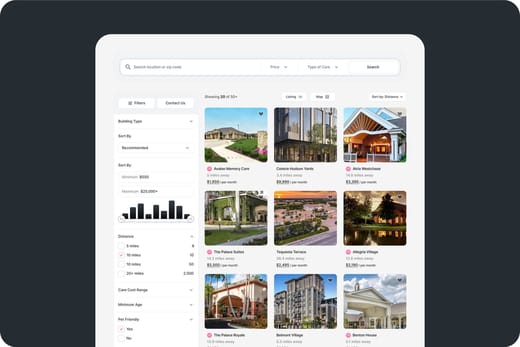
Care Cost Calculator: See Prices in Your Area
Nursing Home Data Explorer
Don’t Wait Too Long: 7 Red Flag Signs Your Parent Needs Assisted Living Now
The True Cost of Assisted Living in 2025 – And How Families Are Paying For It
Understanding Senior Living Costs: Pricing Models, Discounts & Financial Assistance

We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
We'll send you a PDF version of the touring checklist.
