Westridge Health Care Center
Westridge Health Care Center is a Nursing Home in Indiana
Westridge Health Care Center is a Nursing Home in Indiana
Westridge Health Care Center
Westridge Health Care Center is a Nursing Home in Indiana
Westridge Health Care Center is a Nursing Home in Indiana
Experience exceptional care at Westridge Health Care Center, a distinct community in Terre Haute, IN, offering skilled nursing, memory care, and short-term rehabilitation. With a compassionate and well-trained team, residents receive exceptional care for their unique needs around the clock. Medicare and Medicaid are also accepted to ease financial burdens.
To enhance residents’ living experiences, physical, occupational, and speech therapy services are conducted. Healthy meals are important for residents’ well-being, so delicious and well-balanced meals are provided to meet their dietary needs and preferences. The community’s wide range of care options and state-of-the-art amenities ensures residents reach beyond their potential in retirement.
-
The property runs a smaller bed inventory than most peers, focusing on a more intimate census. Residents tend to stay here longer than similar facilities across the state.
-
Home revenue sits below most peers, indicating modest billing throughput. Payroll costs fall below most facilities, hinting at lean staffing budgets. Total income mirrors statewide norms, reflecting a balanced margin profile.
-
Medicare nights track the statewide midpoint, keeping volumes steady. Medicaid nights fall below most peers, pointing to lighter Medicaid reliance. Private pay nights trail most peers, signaling limited market-rate volume.
 Percentage of home revenue spent on payroll costs.
Percentage of home revenue spent on payroll costs.
 CMS 5-star rating based on health inspections, staffing, and quality measures.
CMS 5-star rating based on health inspections, staffing, and quality measures.
 Rating based on deficiencies found during state health inspections.
Rating based on deficiencies found during state health inspections.
 Rating based on nurse staffing hours per resident per day.
Rating based on nurse staffing hours per resident per day.
 Quality Measures rating based on clinical outcomes for residents.
Quality Measures rating based on clinical outcomes for residents.
 Total nurse staffing hours per resident per day.
Total nurse staffing hours per resident per day.
 Number of resident nights paid by Medicare for short-term or rehab care.
Number of resident nights paid by Medicare for short-term or rehab care.
 Resident nights covered by Medicaid for long-term care or support services.
Resident nights covered by Medicaid for long-term care or support services.
 Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Nights paid privately by residents or families, without Medicare/Medicaid coverage.
How BBB ratings work
About this community
Indiana average: 68%
Additional licensing details
Ownership & operating entity
Westridge Health Care Center is legally operated by BOARD OF TRUSTEES OF THE FLAVIUS J WITHAM MEMORIAL, and administrated by LISA BLOESING.
Type Of Units
Staffing
Key information about the people who lead and staff this community.
Leadership
Contact Information
What does this home offer?
Accept Medicaid: Yes
Building Type: Single-story
Dining Services
Housekeeping Services
On-site Medical Care and Health Services
Types of Care at Westridge Health Care Center
Inspection History
In Indiana, the Department of Health, Division of Long Term Care is the primary regulatory body that performs onsite inspections and quality of care reviews for all licensed facilities.
11 visits/inspections
14 visits/inspections triggered by complaints
Results
4 with citations
7 without citations
Indiana average: 11 complaint visits
3 complaints
Formal expressions of dissatisfaction or concern made by residents, or their families regarding various aspects of the care, services, and environment provided.
Indiana average: 4 complaints
29 citations
Citations indicate regulatory violations. A higher number implies the facility had several areas requiring improvement.
Indiana average: 19 citations
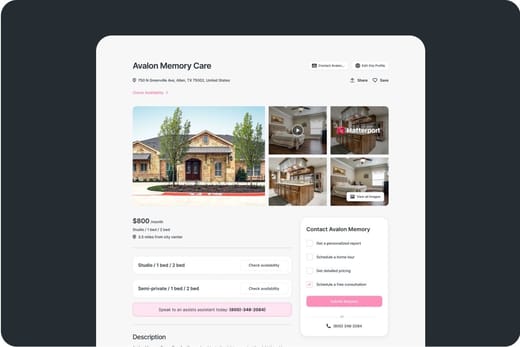
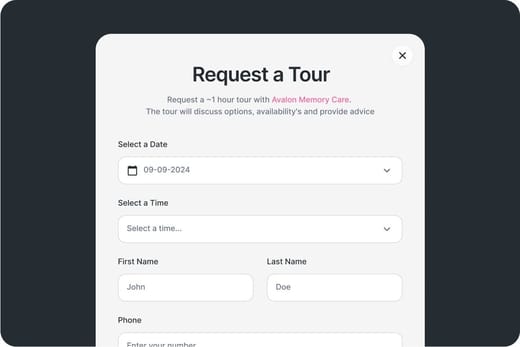
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.
Places of interest near Westridge Health Care Center
2.8 miles from city center
125 W Margaret Ave, Terre Haute, IN 47802
Calculate Travel Distance to Westridge Health Care Center
Add your location
Comparison Chart
The information below is reported by the Indiana Department of Health, Division of Long Term Care.24/7 care needed
24/7 care needed
24/7 care needed
24/7 care needed
24/7 care needed
Staffing Data
Source: CMS Payroll-Based Journal (Q2 2025)
Nursing Staff Breakdown
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 11 | 7.1 | Yes |
| Licensed Practical Nurse | 5 | 7.4 | Yes |
| Certified Nursing Assistant | 18 | 7 | No |
Staff by Category
Contractor Analysis
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 18 | 0 | 18 | 5,768 | 91 | 100% | 7 |
| Licensed Practical Nurse | 4 | 1 | 5 | 2,083 | 91 | 100% | 7.4 |
| Medication Aide/Technician | 8 | 1 | 9 | 2,078 | 91 | 100% | 7.9 |
| Registered Nurse | 7 | 4 | 11 | 1,596 | 87 | 96% | 7.1 |
| Qualified Activities Professional | 0 | 3 | 3 | 1,115 | 90 | 99% | 12.3 |
| Nurse Aide in Training | 3 | 0 | 3 | 993 | 64 | 70% | 8 |
| Physical Therapy Aide | 0 | 1 | 1 | 577 | 76 | 84% | 7.6 |
| Nurse Practitioner | 1 | 0 | 1 | 529 | 66 | 73% | 8 |
| Administrator | 1 | 0 | 1 | 480 | 60 | 66% | 8 |
| Other Dietary Services Staff | 1 | 0 | 1 | 310 | 59 | 65% | 5.3 |
| Qualified Social Worker | 0 | 2 | 2 | 216 | 61 | 67% | 2.8 |
| Respiratory Therapy Technician | 0 | 2 | 2 | 93 | 44 | 48% | 1.8 |
| Physical Therapy Assistant | 0 | 1 | 1 | 58 | 24 | 26% | 2.4 |
| Occupational Therapy Aide | 0 | 1 | 1 | 27 | 6 | 7% | 4.5 |
| Occupational Therapy Assistant | 0 | 1 | 1 | 21 | 3 | 3% | 6.9 |
| Medical Director | 0 | 1 | 1 | 12 | 5 | 5% | 2.4 |
Health Inspection History
Source: CMS Health Citations (Apr 2023 – Sep 2025)
Citation Severity Distribution
Top Deficiency Categories
Citation Sources
State Comparison (IN)
Recent Citations (Last 3 Years)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Sep 19, 2025 | D | Infection Control | F0880 | Corrected |
| Sep 19, 2025 | D | Nursing Services | F0726 | Corrected |
| Mar 20, 2025 | D | Infection Control | F0880 | Corrected |
| Mar 20, 2025 | D | Nutrition | F0812 | Corrected |
| Mar 20, 2025 | D | Pharmacy | F0761 | Corrected |
| Mar 20, 2025 | D | Care Planning | F0842 | Corrected |
| Mar 20, 2025 | D | Resident Rights | F0561 | Corrected |
| Jun 06, 2024 | E | Care Planning | F0657 | Corrected |
| Mar 01, 2024 | E | Infection Control | F0880 | Corrected |
| Mar 01, 2024 | D | Nutrition | F0812 | Corrected |
| Mar 01, 2024 | D | Quality of Care | F0688 | Corrected |
| Mar 01, 2024 | D | Care Planning | F0659 | Corrected |
| Mar 01, 2024 | D | Resident Rights | F0558 | Corrected |
| Apr 17, 2023 | D | Nursing Services | F0726 | Corrected |
| Apr 17, 2023 | D | Nutrition | F0812 | Corrected |
| Apr 17, 2023 | D | Pharmacy | F0757 | Corrected |
| Apr 17, 2023 | D | Pharmacy | F0761 | Corrected |
| Apr 17, 2023 | D | Quality of Care | F0690 | Corrected |
| Apr 17, 2023 | D | Quality of Care | F0695 | Corrected |
| Apr 17, 2023 | D | Care Planning | F0656 | Corrected |
| Apr 17, 2023 | D | Care Planning | F0657 | Corrected |
| Apr 17, 2023 | D | Care Planning | F0842 | Corrected |
Facility Characteristics
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Resident Census by Payment Source
Programs & Services
Family Engagement
Active councils help families stay involved in care decisions and facility operations.
Quality Measures
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Long-Stay Resident Measures
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Short-Stay Resident Measures
Measures for residents who stay 100 days or less (typically rehabilitation patients).

Guides for Better Senior Living
From costs to care, explore the most important topics to make informed decisions about your future.
Claim What’s Yours: Financial Aid for Indiana Seniors
- General: Age 65+ or disabled, Indiana resident, Medicaid-eligible, nursing home-level care need.
- Income Limits (2025): ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- IN Specifics: Requires level-of-care determination.
- Services: Personal care (5-7 hours/day), respite (240 hours/year), adult day care (~$60/day), home health services.
- General: Age 60+, Indiana resident, at risk of nursing home.
- Income Limits: ~$2,000/month (varies).
- Asset Limits: $10,000 (individual).
- IN Specifics: Limited funding; regional variation.
- Services: In-home care (3-5 hours/week), respite (up to 10 days/year), transportation (~5 trips/month).
- General: Age 65+, or blind, or disabled, Indiana resident, in approved facility, low-income or SSI recipient.
- Income Limits (2025): ~$1,004/month (including SSI).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- IN Specifics: ~50 facilities statewide; per diem rate set by FSSA.
- Services: Room/board, laundry, minimal care coordination (~$20-$50/day subsidy).
- General: Age 65+ or disabled, Indiana resident, Medicare Part A/B.
- Income Limits (2025): ~$2,510/month (QMB), ~$3,380/month (SLMB), ~$3,598/month (QI)—individual.
- Asset Limits: $9,430 (individual), $14,130 (couple).
- IN Specifics: Three tiers; no waitlist.
- Services: Covers Part B premiums ($174.70/month), deductibles ($240/year), copays (~20%).
- General: Caregivers of 60+ needing care or 55+ caregivers of others; Indiana resident; functional needs (2+ ADLs).
- Income Limits (2025): Prioritizes ~$24,980/year (individual); no strict cap.
- Asset Limits: Not assessed; need-based.
- IN Specifics: 16 AAAs; prioritizes low-income, rural caregivers.
- Services: Respite (4-6 hours/week or 5 days/year), adult day care ($60/day), caregiver training.
- General: Age 55+, unemployed, low-income, Indiana resident.
- Income Limits (2025): ~$1,983/month (125% FPL).
- Asset Limits: Not specified; income-focused.
- IN Specifics: Priority for veterans, rural residents.
- Services: Paid training (~20 hours/week at ~$7.25/hour), job placement.
- General: Age 65+ or disabled veteran/spouse, Indiana resident, wartime service, need for ADL help (A&A) or homebound.
- Income Limits (2025): Net income < ~$1,984/month (veteran with dependent, A&A); pension offsets income.
- Asset Limits: ~$155,356 (net worth limit).
- IN Specifics: High veteran demand statewide.
- Services: Cash (~$1,433-$2,642/month veteran, ~$951-$1,318 spouse) for care costs (e.g., in-home, assisted living).
Contact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today