Fairlawn Health and Rehabilitation of Cascadia
Fairlawn Health and Rehabilitation of Cascadia is a Nursing Home in Oregon
Fairlawn Health and Rehabilitation… is a Nursing Home in Oregon
Fairlawn Health and Rehabilitation of Cascadia
Fairlawn Health and Rehabilitation of Cascadia is a Nursing Home in Oregon
Fairlawn Health and Rehabilitation… is a Nursing Home in Oregon
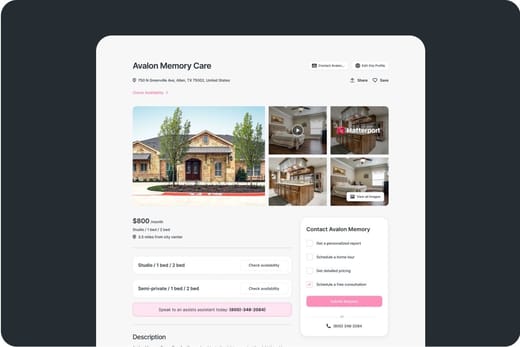
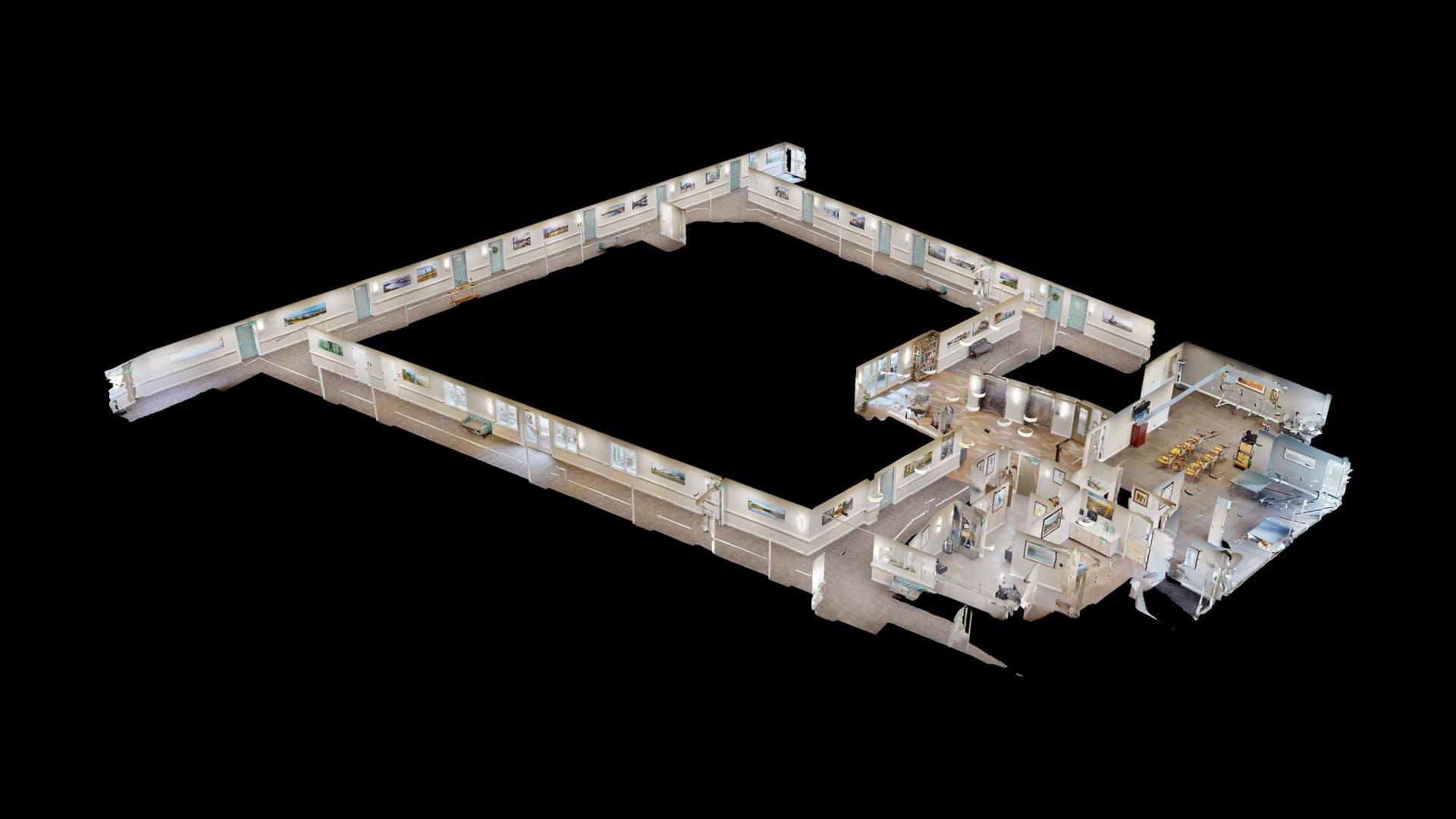
Fairlawn Health and Rehabilitation of Cascadia provides one of Gresham’s most trusted nursing homes. The center has a professional staff committed to providing all seniors with a safe and comfortable environment. With its professional approach, the nursing home aims to change the meaning of skilled nursing and rehabilitation for seniors through the exceptional care delivered by the compassionate staff.
The upscale nursing homes provide state-of-the-art features that cater to short-term or long-term residents; they are also guaranteed to feel comfortable and know that they belong in a home that offers 24-hour nursing care with specialized programs such as therapies in a resort-like community.
-
This nursing home maintains occupancy well above most state peers, signaling sustained demand. Bed capacity aligns with the typical community size in the state, allowing steady admissions. Residents tend to stay here longer than similar facilities across the state.
-
Home revenue ranks in the upper tier statewide, reflecting strong billing volume. Payroll spending sits in the top tier, showing a strong investment in staffing resources. Total income exceeds the majority of state facilities, highlighting strong profitability.
-
Medicare nights run higher than most peers, indicating robust short-stay referrals. Medicaid nights are roughly in line with the state middle third, maintaining a balanced safety-net share. Private pay nights lead the state, showing strong demand from market-rate residents.
 Percentage of home revenue spent on payroll costs.
Percentage of home revenue spent on payroll costs.
 CMS 5-star rating based on health inspections, staffing, and quality measures.
CMS 5-star rating based on health inspections, staffing, and quality measures.
 Rating based on deficiencies found during state health inspections.
Rating based on deficiencies found during state health inspections.
 Rating based on nurse staffing hours per resident per day.
Rating based on nurse staffing hours per resident per day.
 Quality Measures rating based on clinical outcomes for residents.
Quality Measures rating based on clinical outcomes for residents.
 Total nurse staffing hours per resident per day.
Total nurse staffing hours per resident per day.
 Number of resident nights paid by Medicare for short-term or rehab care.
Number of resident nights paid by Medicare for short-term or rehab care.
 Resident nights covered by Medicaid for long-term care or support services.
Resident nights covered by Medicaid for long-term care or support services.
 Nights paid privately by residents or families, without Medicare/Medicaid coverage.
Nights paid privately by residents or families, without Medicare/Medicaid coverage.
About this community
Additional licensing details
Ownership & operating entity
Fairlawn Health and Rehabilitation of Cascadia is legally operated by Gresham of Cascadia, LLC, and administrated by Leslie Workman.
Care Services
Contact Information
Additional Policies & Features
Access & Eligibility
Ways to qualify for care at this community, including accepted programs and payment options.
This facility is certified for eligible Medicaid services.
This facility is certified for eligible Medicare services.
Inspection History
In Oregon, the Department of Human Services, Aging and People with Disabilities performs unannounced surveys and regular inspections to ensure resident safety in all care settings.
10 visits/inspections
Latest inspection
10 licensing violations
Violations of state licensing requirements identified during facility inspections.
11 deficiencies
Deficiencies indicate regulatory issues. A higher number implies the facility had several areas requiring improvement.
Comparison Chart
The information below is reported by the Oregon Department of Human Services, Aging and People with Disabilities.For seniors needing help with daily tasks but not full-time nursing.
For seniors needing help with daily tasks but not full-time nursing.
For seniors needing help with daily tasks but not full-time nursing.
Specialized care for those with Memory Loss, Alzheimer's, or dementia, ensuring safety and support.
For seniors needing help with daily tasks but not full-time nursing.
For seniors needing help with daily tasks but not full-time nursing.
Hospice Care
For self-sufficient seniors seeking community and minimal assistance.
24/7 care needed
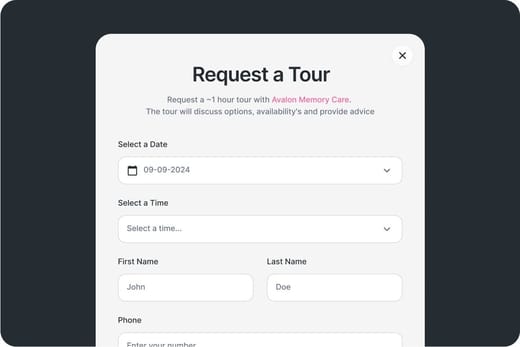
Touring Checklist for Senior Living
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
Location
Community Spaces and Overall Environment
Services
Staffing
Accommodations
Finances
Other Notes
Send Checklist to Your Email
We'll send you a PDF version of the touring checklist.
Places of interest near Fairlawn Health and Rehabilitation of Cascadia
1.9 miles from city center
3457 NE Division St, Gresham, OR 97030
Calculate Travel Distance to Fairlawn Health and Rehabilitation of Cascadia
Add your location
Staffing Data
Source: CMS Payroll-Based Journal (Q2 2025)
Nursing Staff Breakdown
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 16 | 10.5 | Yes |
| Licensed Practical Nurse | 7 | 9.8 | Yes |
| Certified Nursing Assistant | 83 | 7.8 | Yes |
Staff by Category
Contractor Analysis
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 63 | 20 | 83 | 16,247 | 91 | 100% | 7.8 |
| Registered Nurse | 11 | 5 | 16 | 4,195 | 91 | 100% | 10.5 |
| Licensed Practical Nurse | 6 | 1 | 7 | 2,870 | 89 | 98% | 9.8 |
| Medication Aide/Technician | 7 | 0 | 7 | 2,693 | 91 | 100% | 9 |
| Physical Therapy Assistant | 5 | 0 | 5 | 850 | 80 | 88% | 5.2 |
| Respiratory Therapy Technician | 3 | 0 | 3 | 699 | 79 | 87% | 7.4 |
| Mental Health Service Worker | 1 | 0 | 1 | 525 | 65 | 71% | 8.1 |
| Administrator | 1 | 0 | 1 | 512 | 64 | 70% | 8 |
| Nurse Practitioner | 1 | 0 | 1 | 512 | 64 | 70% | 8 |
| Dietitian | 1 | 0 | 1 | 454 | 59 | 65% | 7.7 |
| Speech Language Pathologist | 1 | 0 | 1 | 376 | 43 | 47% | 8.7 |
| Qualified Social Worker | 1 | 0 | 1 | 365 | 63 | 69% | 5.8 |
| Occupational Therapy Aide | 0 | 1 | 1 | 128 | 37 | 41% | 3.5 |
| Occupational Therapy Assistant | 0 | 3 | 3 | 41 | 51 | 56% | 0.8 |
| Clinical Nurse Specialist | 1 | 0 | 1 | 36 | 5 | 5% | 7.2 |
| Dental Services Staff | 1 | 0 | 1 | 13 | 2 | 2% | 6.7 |
| Other Dietary Services Staff | 1 | 0 | 1 | 11 | 2 | 2% | 5.3 |
| Medical Director | 0 | 1 | 1 | 2 | 2 | 2% | 0.8 |
Health Inspection History
Source: CMS Health Citations (May 2018 – Dec 2024)
Citation Severity Distribution
Top Deficiency Categories
Citation Sources
State Comparison (OR)
Recent Citations (Last 3 Years)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Dec 06, 2024 | E | Nutrition | F0812 | Corrected |
| Dec 06, 2024 | D | Quality of Care | F0689 | Corrected |
| Dec 06, 2024 | D | Quality of Care | F0690 | Corrected |
| Dec 06, 2024 | D | Care Planning | F0660 | Corrected |
| Dec 06, 2024 | D | Resident Rights | F0584 | Corrected |
| Nov 21, 2024 | D | Quality of Care | F0684 | Corrected |
| Nov 21, 2024 | D | Care Planning | F0661 | Corrected |
| May 24, 2024 | D | Quality of Care | F0684 | Corrected |
| Oct 18, 2023 | D | Pharmacy | F0760 | Corrected |
| Aug 29, 2023 | D | Quality of Care | F0684 | Corrected |
| Jan 30, 2023 | G | Quality of Care | F0684 | Corrected |
| Jan 21, 2020 | D | Infection Control | F0880 | Corrected |
| Jan 21, 2020 | E | Nursing Services | F0732 | Corrected |
| Jan 21, 2020 | E | Nutrition | F0804 | Corrected |
| Jan 21, 2020 | F | Nutrition | F0812 | Corrected |
| Jan 21, 2020 | D | Pharmacy | F0757 | Corrected |
| Jan 21, 2020 | G | Pharmacy | F0760 | Corrected |
| Jan 21, 2020 | D | Quality of Care | F0679 | Corrected |
| Jan 21, 2020 | D | Quality of Care | F0689 | Corrected |
| Jan 21, 2020 | D | Quality of Care | F0690 | Corrected |
| Jan 21, 2020 | D | Care Planning | F0636 | Corrected |
| Jan 21, 2020 | D | Care Planning | F0656 | Corrected |
| Jan 21, 2020 | E | Resident Rights | F0577 | Corrected |
| Jan 21, 2020 | D | Resident Rights | F0578 | Corrected |
| Jan 21, 2020 | D | Resident Rights | F0580 | Corrected |
| May 14, 2018 | D | Pharmacy | F0758 | Corrected |
| May 14, 2018 | D | Care Planning | F0660 | Corrected |
Facility Characteristics
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Resident Census by Payment Source
Programs & Services
Family Engagement
Active councils help families stay involved in care decisions and facility operations.
Quality Measures
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Long-Stay Resident Measures
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Short-Stay Resident Measures
Measures for residents who stay 100 days or less (typically rehabilitation patients).

Guides for Better Senior Living
From costs to care, explore the most important topics to make informed decisions about your future.
Claim What’s Yours: Financial Aid for Oregon Seniors
- General: Age 60+, Oregon resident, at risk of nursing home but not Medicaid-eligible.
- Income Limits: ~$2,000/month (individual, varies).
- Asset Limits: $5,000 (individual).
- OR Specifics: Cost-sharing required; rural/urban balance.
- Services: In-home care (3-5 hours/week), respite (up to 10 days/year), adult day care (~$70/day), transportation (~5 trips/month).
- General: Age 65+ or disabled, Oregon resident, Medicaid-eligible, nursing home-level care need.
- Income Limits (2025): ~$2,829/month (300% FBR, individual).
- Asset Limits: $2,000 (individual), $3,000 (couple).
- OR Specifics: High demand in urban areas (e.g., Portland).
- Services: Personal care (5-7 hours/day), respite (240 hours/year), adult day care ($70/day), home modifications ($1,500 avg.).
- General: Age 55+, OR resident (specific counties), NFLOC, safe with PACE support.
- Income Limits (2025): ~$2,829/month (Medicaid-eligible); private pay option available.
- Asset Limits: $2,000 (individual), $3,000 (couple) for Medicaid enrollees.
- OR Specifics: Available in 11 counties (e.g., Multnomah, Washington); Providence ElderPlace dominant provider.
- Services: Personal care (5-7 hours/day), medical care, meals, transportation, respite, therapies.
- General: Age 65+ or disabled, OR resident, Medicare Part A/B.
- Income Limits (2025): ~$2,510/month (QMB), ~$3,380/month (SLMB), ~$3,598/month (QI)—individual.
- Asset Limits: $9,430 (individual), $14,130 (couple).
- OR Specifics: Three tiers; includes Extra Help for Part D; no waitlist.
- Services: Covers Part B premiums ($174.70/month), deductibles ($240/year), copays (~20%).
- General: Age 60+ prioritized, OR resident, low-income household.
- Income Limits (2025): ~$3,970/month (individual, 185% FPL).
- Asset Limits: Not assessed; income-focused.
- OR Specifics: Covers gas, electric, oil; emergency aid via Oregon Energy Fund (OEF).
- Services: Heating/cooling aid ($300-$1,000/season), emergency aid ($500 max via OEF).
- General: Caregivers of 60+ needing care or 55+ caregivers of others; OR resident; functional needs (2+ ADLs).
- Income Limits (2025): No strict cap; prioritizes low-income (~$24,980/year).
- Asset Limits: Not assessed; need-based.
- OR Specifics: 15 regions; rural priority; includes grandparent caregivers.
- Services: Respite (4-6 hours/week or 5 days/year), adult day care ($60/day), training, supplies (~$500/year).
- General: Age 55+, unemployed, low-income, OR resident.
- Income Limits (2025): ~$1,983/month (125% FPL).
- Asset Limits: Not specified; income-focused.
- OR Specifics: Priority for veterans, rural residents; Easterseals/AARP partnership.
- Services: Paid training (~20 hours/week at ~$7.25/hour), job placement.
- General: Age 65+ or disabled veteran/spouse, OR resident, wartime service, need for ADL help (A&A) or homebound.
- Income Limits (2025): Net income < ~$1,984/month (veteran with dependent, A&A); pension offsets income.
- Asset Limits: ~$155,356 (net worth limit).
- OR Specifics: High veteran demand; Oregon Veterans’ Homes option.
- Services: Cash (~$1,433-$2,642/month veteran, ~$951-$1,318 spouse) for care costs (e.g., in-home, assisted living).
- General: Age 62+, OR resident, homeowner 5+ years, low-income.
- Income Limits (2025): ~$58,000/year (household, adjusted annually).
- Asset Limits: Home value < county median; equity > 15%.
- OR Specifics: Deferred taxes accrue 6% interest; repaid upon sale/death.
- Services: Tax deferral (~$1,000-$3,000/year avg., varies by county).
- General: Age 60+, OR resident (or spouse of any age); no income limit.
- Income Limits (2025): None; donations encouraged.
- Asset Limits: Not assessed.
- OR Specifics: Includes Meals on Wheels; prioritizes homebound/low-income.
- Services: Home-delivered or congregate meals (~$5-$7/meal value, 5 meals/week avg.).
Contact Us

Your Senior Care Partner, Every Step of the Way
We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today