Mix of rehab and long-term care
This home supports both short-term rehab and long-term care, with residents staying for a wide range of durations.
We arrange tours, appointments, and even moving support so you don’t have to
Found amidst Gainesville, Florida, the Terrace Health & Rehabilitation Center presents itself as a haven of skilled rehabilitation and nursing care. With a spacious and welcoming atmosphere, this center prioritizes the comfort and well-being of its senior residents. Its strategic location near renowned hospitals adds to the convenience, ensuring easy access to medical facilities and expert healthcare.
Beyond providing top-notch medical services, the center fosters a warm environment of companionship and support. They seamlessly offer both short-term and long-term rehabilitation solutions, catering to the diverse needs of their residents. Whether it’s hospice, palliative care, or respite care, they handle each service with professionalism and compassion, making it an exceptional long-term care facility. Moreover, the center prides itself on an array of engaging activities, from games, movies, and crafts to light exercise classes.
Barry Audain is a Licensed Nursing Home Administrator with over 8 years of long-term care experience across Georgia and Florida. He holds degrees in Kinesiology and Health Care Administration. Barry’s background as a Certified Nursing Assistant and his expertise in financial administration, regulatory compliance, and quality assurance reflect his deep commitment to quality care for the elderly community at Terrace Health & Rehabilitation Center.
Offers a balance of services and community atmosphere.
Occupancy is moderate, suggesting balanced demand.
This home supports both short-term rehab and long-term care, with residents staying for a wide range of durations.
32% of new residents, usually for short-term rehab.
56% of new residents, often for short stays.
11% of new residents, often for long-term daily care.
 The portion of the home's budget spent on staff, including nurses, caregivers, and other employees who support care and operations.
The portion of the home's budget spent on staff, including nurses, caregivers, and other employees who support care and operations.
 All remaining costs needed to run the home, such as food, utilities, building maintenance, supplies and administrative expenses.
All remaining costs needed to run the home, such as food, utilities, building maintenance, supplies and administrative expenses.
Nursing Homes 24/7 care needed
Respite Care
Hospice Care
Nursing Homes 24/7 care needed
Respite Care
Nursing Homes 24/7 care needed
Nursing Homes 24/7 care needed
Hospice Care
Nursing Homes 24/7 care needed
Respite Care
8.0 miles from city center
7207 SW 24th Ave, Gainesville, FL 32607
Add your location
Source: CMS Payroll-Based Journal (Q2 2025)
| Role ⓘ | Count ⓘ | Avg Shift (hrs) ⓘ | Uses Contractors? ⓘ |
|---|---|---|---|
| Registered Nurse | 13 | 7 | No |
| Licensed Practical Nurse | 43 | 7.5 | No |
| Certified Nursing Assistant | 114 | 7.4 | Yes |
| Role ⓘ | Employees ⓘ | Contractors ⓘ | Total Staff ⓘ | Total Hours ⓘ | Days Worked ⓘ | % of Days ⓘ | Avg Shift (hrs) ⓘ |
|---|---|---|---|---|---|---|---|
| Certified Nursing Assistant | 113 | 1 | 114 | 28,068 | 91 | 100% | 7.4 |
| Licensed Practical Nurse | 43 | 0 | 43 | 10,760 | 91 | 100% | 7.5 |
| RN Director of Nursing | 10 | 0 | 10 | 4,384 | 91 | 100% | 8.4 |
| Speech Language Pathologist | 10 | 0 | 10 | 3,470 | 69 | 76% | 7.5 |
| Registered Nurse | 13 | 0 | 13 | 2,145 | 90 | 99% | 7 |
| Physical Therapy Assistant | 5 | 0 | 5 | 1,761 | 79 | 87% | 8 |
| Physical Therapy Aide | 6 | 0 | 6 | 1,466 | 68 | 75% | 7.4 |
| Qualified Social Worker | 4 | 0 | 4 | 1,058 | 66 | 73% | 6.1 |
| Clinical Nurse Specialist | 6 | 0 | 6 | 907 | 74 | 81% | 6.9 |
| Dietitian | 3 | 0 | 3 | 896 | 77 | 85% | 7.5 |
| Respiratory Therapy Technician | 7 | 0 | 7 | 794 | 77 | 85% | 5.6 |
| Nurse Practitioner | 2 | 0 | 2 | 536 | 57 | 63% | 8 |
| Administrator | 1 | 0 | 1 | 520 | 65 | 71% | 8 |
| Mental Health Service Worker | 1 | 0 | 1 | 472 | 59 | 65% | 8 |
| Nurse Aide in Training | 1 | 0 | 1 | 108 | 13 | 14% | 8.3 |
| Medical Director | 0 | 1 | 1 | 52 | 26 | 29% | 2 |
Source: CMS Health Citations (Jan 2022 – Oct 2024)
| Date | Severity ? | Category | Tag | Status |
|---|---|---|---|---|
| Oct 04, 2024 | D | Infection Control | F0880 | Corrected |
| Oct 04, 2024 | D | Quality of Care | F0684 | Corrected |
| Oct 04, 2024 | D | Care Planning | F0656 | Corrected |
| Oct 04, 2024 | D | Care Planning | F0842 | Corrected |
| Apr 26, 2024 | D | Resident Rights | F0573 | Corrected |
| Jun 07, 2023 | D | Infection Control | F0880 | Corrected |
| Jun 07, 2023 | E | Nutrition | F0812 | Corrected |
| Jun 07, 2023 | D | Pharmacy | F0761 | Corrected |
| Jun 07, 2023 | E | Quality of Care | F0684 | Corrected |
| Jun 07, 2023 | D | Quality of Care | F0695 | Corrected |
| Jun 07, 2023 | E | Care Planning | F0842 | Corrected |
| Mar 06, 2023 | C | Nursing Services | F0732 | Corrected |
| Jan 21, 2022 | F | Nutrition | F0812 | Corrected |
| Jan 21, 2022 | F | Pharmacy | F0761 | Corrected |
| Jan 21, 2022 | D | Quality of Care | F0684 | Corrected |
| Jan 21, 2022 | D | Quality of Care | F0695 | Corrected |
Source: CMS Long-Term Care Facility Characteristics (Data as of Jan 2026)
Active councils help families stay involved in care decisions and facility operations.
CMS quality measures assess care quality for long-stay and short-stay residents. Lower percentages generally indicate better outcomes for most measures.
Source: CMS Nursing Home Compare (Data as of Jan 2026)
Composite score based on pressure ulcers, falls with injury, weight loss, walking ability decline, and ADL decline
Composite score based on ADL decline, walking ability decline, and incontinence
Measures for residents who stay 101 days or more. For most measures, lower percentages indicate better care.
Measures for residents who stay 100 days or less (typically rehabilitation patients).
Federal penalties imposed by CMS for regulatory violations, including civil money penalties (fines) and denials of payment for new Medicare/Medicaid admissions.
Source: CMS Penalties Database (Data as of Jan 2026)
Showing all 1 penalties (Jan 2024 - Jan 2024)
Historical financial and operational data for Terrace Health & Rehabilitation Center based on CMS SNF Cost Reports.
Loading trend charts...
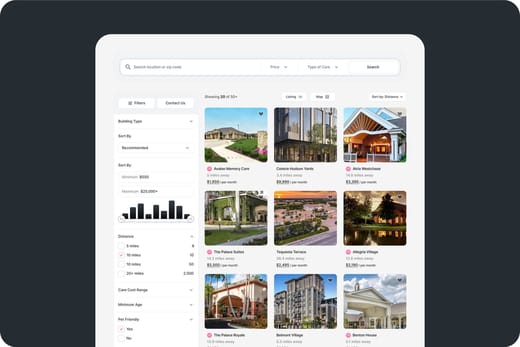
Care Cost Calculator: See Prices in Your Area
Nursing Home Data Explorer
Don’t Wait Too Long: 7 Red Flag Signs Your Parent Needs Assisted Living Now
The True Cost of Assisted Living in 2025 – And How Families Are Paying For It
Understanding Senior Living Costs: Pricing Models, Discounts & Financial Assistance

We help families find affordable senior communities and unlock same day discounts, Medicaid, and Medicare options tailored to your needs.
Contact us Today
Touring a community? Use this expert-backed checklist to stay organized, ask the right questions, and find the perfect fit.
We'll send you a PDF version of the touring checklist.
