Recovering from a hospital stay is crucial for maintaining older adults’ well-being. Whether the hospitalization is due to a surgery, injury, illness, or a complex medical condition like stroke or heart attack, rehabilitation would help older adults regain their health and independence. Rehabilitation may also lessen the risk for rehospitalization and is often provided in settings like skilled nursing facilities (SNFs), assisted living communities, inpatient rehabilitation facilities (IRFs), and at home with in-home through in-home care. To ensure the right care is received, it is better to know the options available according to older adults’ medical needs, functional abilities, budget, and preferences. Utilizing data from the Genworth Cost of Care Survey 2025, Medicare.gov, and the U.S. News & World Report, this article explores the best rehabilitation options.
What is Senior Rehabilitation?
Senior rehabilitation, also known as post-acute care, focuses on the physical, cognitive, and functional challenges of older adults, providing necessary medical support and therapies to maintain their independence and improve their conditions. There’s a wide range of reasons for rehabilitation, with the following as the most common:
- Musculoskeletal issues – Hip or knee injury and fractures.
- Neurological events – Traumatic brain injuries and strokes.
- Cardiac conditions – Bypass surgery and heart attack.
- Infections – Pneumonia, sepsis, and gastrointestinal infections.
Rehabilitation usually specializes in providing care after a hospital stay and aims to reduce older adults’ pain and discomfort.
Care Options
Various care providers offer rehabilitation, catering to older adults’ needs and goals. The following shows the primary options, services provided, and suitable candidates.
- Skilled Nursing Facilities (SNFs)
- Provides round-the-clock nursing care and rehabilitation for those needing intensive medical care after hospitalization. Often include short-term stays, ranging from days to weeks, in a clinical, hospital-like environment with private or shared accommodations.
- Services
- All forms of therapy, including physical, which aims to enhance mobility; occupational that focuses on ADLs and motor skills; and speech therapy, which focuses on cognitive issues, communication, and swallowing problems.
- Medical care, such as wound care, IV medications, and medication management.
- Tailored dietary plans, approved by licensed dietitians.
- Social Services, including counseling and discharge planning, as noted by the Centers Health Care.
- Duration: Usually 1 to 4 weeks; Medicare can cover up to 10 days.
- Pros
- Intensive medical care
- Comprehensive therapy programs typically last one to two hours a day.
- Expenses covered by Medicare
- Cons
- Often, a hospital-like setting, which lacks a social environment, in contrast to assisted living.
- Best for older adults with complex medical needs or those who are unable to stay at home due to a lack of support and mobility issues.
- Inpatient Rehabilitation Facilities (IRFs)
- Provides intensive therapy, usually lasts three hours a day, five days a week, and coordinates with physicians, therapists, and nurses to align care for older adults. IRFs can be a standalone community or part of a hospital.
- Services
- Rigorous physical, occupational, and speech therapies.
- Physician-led care plans for complex medical conditions, like stroke and spinal cord injury.
- Nursing support for medication management and wound care.
- Duration: Typically one to three weeks, depending on recovery.
- Pros
- Quick recovery due to high-intensity therapy.
- Comprehensive care from multidisciplinary teams.
- Qualifying diagnoses can be covered by Medicare Part A.
- Cons
- An intensive therapy schedule can be exhausting.
- Higher costs due to limited coverage from government services.
- Lack of social activities.
- Ideal for older adults with serious conditions who need intensive rehabilitation to regain function.
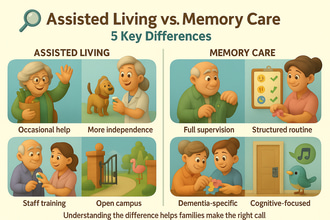
- Assisted Living Communities
- Short-term rehabilitation, respite stays, and therapy can be provided alongside ADL support in some assisted living communities. Usually promotes a home-like and social environment through communal dining and a calendar of activities.
- Services
- Physical, occupational, and speech therapies are provided through on-site rooms or in collaboration with home health agencies.
- 24/7 ADL support
- Medication management and limited nursing care,
- Social activities
- Duration: Ranging from a few days to several months, often used to bridge home and long-term care.
- Pros
- Community-focused, home-like environment.
- Flexible care plans and stay options.
- Promotes socialization and engagement.
- Cons
- Less medical support than SNFs
- Medicare does not cover room and board.
- Best suited for older adults with moderate needs, but are not yet ready to return home.
- Home Health Care
- Care is provided at home by licensed professionals, like nurses and therapists. Often include rehabilitation services, allowing older adults to recover in a familiar setting.
- Services
- Physical, occupational, and speech therapies are typically two to three times a week.
- Nursing support for wound care, injections, and vital monitoring.
- Equipment setup after home safety assessments.
- Duration: Depending on progress, may take a few weeks to several months.
- Pros
- A familiar environment can lessen stress and infection risks.
- Personalized and flexible schedules.
- Medicare covers expenses, especially if required by physicians.
- Cons
- Limited socialization.
- Requires self-discipline to follow the therapy schedule.
- Ideal for older adults with mild to moderate needs who can handle ADLs with family support.
- Outpatient Rehabilitation
- Requires older adults at home or in assisted living to visit a rehabilitation center for therapy sessions.
- Services
- Physical, occupational, and speech therapies are usually one to three sessions per week.
- No ADL support.
- Access to advanced equipment, like treadmills and resistance machines.
- Duration: Depending on recovery, it ranges from weeks to months.
- Pros
- According to Medicare.gov, therapy is covered by Medicare Part B.
- It can be cost-effective for those with low-intensity needs.
- Cons
- Requires travelling or transportation.
- No 24/7 support or supervision.
- Ideal for those who can travel and with less intensive needs.
Costs of Senior Rehabilitation in 2025
Depending on the state, level of care, and type of facility, costs may vary.
- Skilled Nursing Facilities
- Average Cost – $9,197 per month for a semi-private room or $10,326 per month for a private room.
- Depending on the state, costs range from $5,125 per month, like that of Texas, to $31,512 per month in Alaska.
- Medicare Coverage – Full coverage for 1 to 20 days, supplementary pay of $204 per day for days 21 to 100 in 2025.
- Out-of-Pocket – Personal items are not included in the coverage, as per Medicare.gov.
- Inpatient Rehabilitation Facilities
- Average Cost – $15,000 to $25,000 monthly due to intensive therapy.
- Medicare Coverage – Coverage includes services after a hospital stay, with an estimated $1,600 deductible in 2025 for days 1 to 60, as noted by Medicare.gov.
- Out-of-Pocket – Supplementary pay for extended stays and non-covered services.
- Assisted Living or Short-Term Rehabilitation
- Average Cost – Standard assisted living communities can cost around $5,676 per month, however, additional fees for therapy are charged up to $500 to $2,000 monthly.
- Medicare Coverage – Therapy is covered if physician-required, but not room or board.
- Home Health Care
- Average Cost – $37 per hour, which amounts to $148 for a four-hour visit, and $5,625 per month for five visits per week.
- Medicare Coverage – Doctor-ordered services are fully covered.
- Out-of-Pocket – ADL support and non-medical aid services are not covered by Medicare.
- Outpatient Rehabilitation
- Average Cost – $100 to $300 per session, which can reach up to $1,000 to $3,000 per month for two to three sessions per week.
- Medicare Coverage – According to Medicare.gov, Medicare Part B covers up to 80% of therapy expenses after a $240 deductible in 2025.
Funding Options
- Medicare – Covers SNF after a 3-day hospital stay, IRF, home health, and outpatient therapy, but not room and board for assisted living.
- Medicaid – Eligible older adults with assets less than $2,000 can receive funding for SNF costs.
- Veterans Benefits – $2,300 monthly is provided through the VA Aid and Attendance program.
- Private Insurance – Rehabilitation can be covered by long-term care policies.
- Out-of-Pocket – Centers Health Care notes that savings, home sales, or reverse mortgages can supplement rehabilitation
Benefits
- Improved Recovery
- SNFs and IRFs can lower risks for rehospitalization.
- Therapies aim to provide quick recovery and ease older adults’ pain and discomfort.
- Enhanced Independence
- Older adults can return home through occupational therapy.
- Safety and Supervision
- 24/7 supervision in SNFs and IRFs can prevent risks for falls and complications.
- Social and Emotional Support
- Rehabilitation in assisted living communities provides social interactions.
- Tailored Care
- Personalized care plans are created with multidisciplinary teams.
Considerations
- Medical Needs
- SNFs and IRFs best suit those with complex medical conditions, like stroke, while those who have undergone minor surgery are ideal for home health and assisted living.
- Support at Home
- Home health requires family support, and older adults who live alone may be better off with inpatient care.
- Budget and Insurance
- AARP suggests checking out-of-pocket costs for assisted living and non-covered services, so that you can prepare accordingly.
- Preferences
- SNFs prioritize medical care and provide minimal social interactions, while home health and assisted living promote comfort and familiarity.
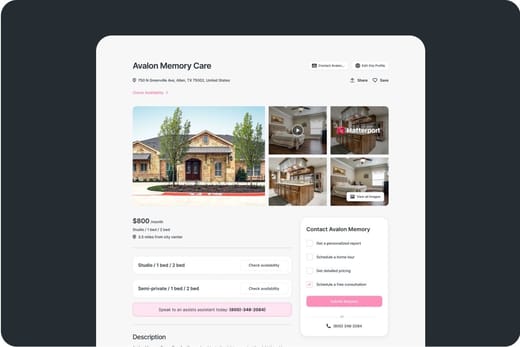
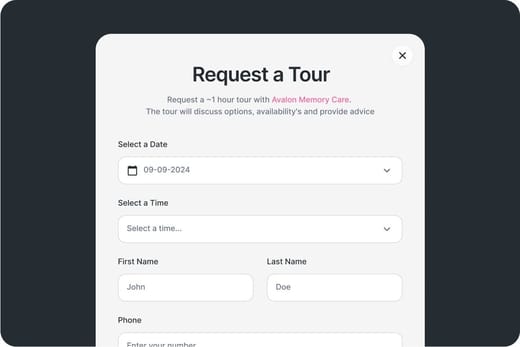
- Facility Quality
- Check for Medicare ratings, team credentials, and amenities provided.
- For better results, touring facilities are also recommended.
Planning Tips
- Create a Discharge Plan: Work closely with the hospital team to create care plans that cater to your needs, including therapy needs and medications.
- Appeal Early Discharge: AARP notes that if an older adult isn’t ready, file an appeal with the hospital or insurer.
- Research in Advance: Identify local SNFs, IRFs, and assisted living communities before a crisis, using Medicare.gov’s Compare tool, per AARP.
- Monitor Care: AARP recommends ensuring medical records and discharge instructions are shared between providers.
- Seek Help: Geriatric care managers or hospital social workers can guide options.
- Prepare the Home: For home health, arrange modifications (e.g., ramps, grab bars) and equipment.
Conclusion
Senior rehabilitation aims to improve older adults’ well-being after hospitalization, and offers several options, including SNFs ($9,197 to $10,326 per month) and IRFs ($15,000 to $25,000 per month), for intensive care, to assisted living ($5,676 per month and additional fees for therapy) and home health care ($5,625 monthly) for moderate needs. Independent older adults may also opt for outpatient rehab, which costs around $1,000 to $3,000 monthly. The best option would depend on the level of care you need and your preferences.