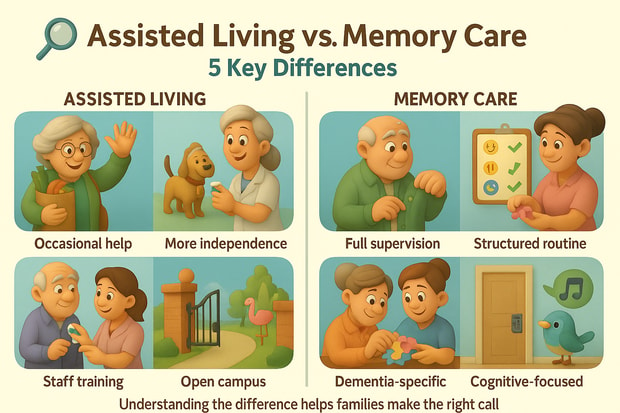
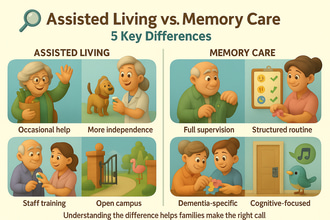
Planning for long-term care requires a better understanding of care options, mainly assisted living and memory care, especially for families looking for care for loved ones with cognitive conditions like Alzheimer’s and dementia. This article explores the main differences between the two options, summarized into five key points, referencing insights from government data and industry standards.
1. Level of Care and Supervision
- Assisted Living
- Assisted living communities mainly help those who need assistance with daily care, including grooming, dressing, bathing, housekeeping, and medication management, while retaining independence. Most assisted living communities focus on maintaining autonomy while supporting physical limitations, as noted by the U.S. Department of Health and Human Services.
- Memory Care
- Specializing in care for cognitive impairments like Alzheimer’s and dementia, memory care communities provide intensive supervision, including round-the-clock monitoring and behavioral management. Structured routines are also provided to ease confusion and agitation and ensure safety. According to the National Center for Assisted Living standards, memory care communities have higher staff-to-resident ratios, with 1:6, in contrast to 1:15 in assisted living.
2. Staff Training and Specialization
- Assisted Living
- Depending on the state, staff are trained to assist with ADLs, help with medication, and coordinate care. The Centers for Medicare & Medicaid Services noted that most states mandate basic caregiving certifications, with 8-16 hours of annual training.
- Memory Care
- Specialized training in dementia and Alzheimer’s care is required, teaching behavior management, communication techniques, and crisis intervention. A minimum of 12 hours of initial training and continuous education is recommended to handle cognitive conditions properly, as per Alzheimer’s Association’s recommendation. Additionally, licensed nurses and therapists are employed in many memory care communities.
3. Facility Design and Environment
- Assisted Living
- According to the U.S. Census Bureau, assisted living communities accommodate up to 20 to 100 residents, focusing on their physical limitations. Most communities utilize apartment-style residences with private and semi-private residences, communal dining areas, and social spaces. Grab bars and wide hallways are also provided for better accessibility.
- Memory Care
- To minimize the effects of dementia symptoms, like agitation and wandering, memory care communities promote a secure and structured environment with gated spaces, locked exits, and color-coded hallways. Adhering to the National Institute on Aging guidelines, memory care units, including those within assisted living communities, accommodate smaller populations, often ranging from 10 to 40 residents.
4. Cost and Funding
- Assisted Living
- Assisted living costs vary by state, however, the national average for assisted living was $4,917 per month, based on the Genworth Cost of Care Survey 2024, with an assumed increase to $5,900 in 2025. Medicare does not cover assisted living, while various states provide Medicaid waivers to offset financial challenges.
- Memory Care
- Genworth reported a median cost of $7,500 to $10,000 for memory care in 2025. As observed, memory care costs more than assisted living due to specialized care and higher staffing needs. To minimize financial burdens, eligible veterans may receive help through the U.S. Department of Veterans Affairs’ Aid and Attendance benefits.
5. Activities and Programming
- Assisted Living
- According to the Administration for Community Living, activities in assisted living communities aim to improve the quality of life of older adults with physical limitations, and often include a wide range of social and recreational activities, like board games, fitness classes, and outings.
- Memory Care
- Memory care programs provide structured routines to improve the cognition of those with cognitive conditions. These activities aim to improve cognition and enhance emotional well-being, and often include music therapy, sensory stimulation, and reminiscence activities. Off-site activities are limited to avoid wandering and ensure safety.
Conclusion
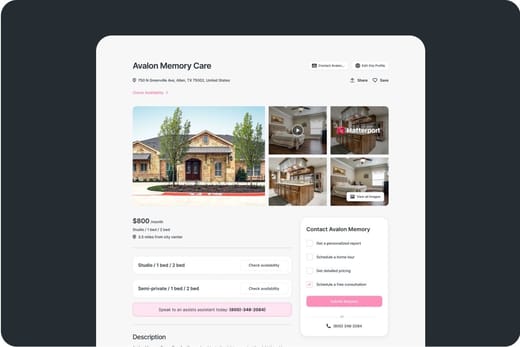
As discussed, the main difference between assisted living and memory care is the focus of care. Assisted living caters to the physical limitations of older adults while aiming to maintain independence and providing assistance with ADLs, and costs around $5,900 per month. In contrast, memory care specializes in the care for those with Alzheimer’s and dementia, providing tailored activities and secure environments, averaging from $7,500 to $10,000 monthly. To ensure that needs are met, it is suggested to plan ahead and assess care needs, budget, and facility options, with the guidance of local agencies and trusted resources like the U.S. Administration on Aging (www.acl.gov). Search for communities here: https://assistedlivingmagazine.com/search/.