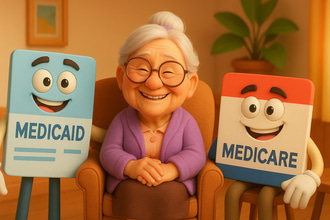
Managing the finances related to assisted living can be overwhelming, especially when looking for resources that can help alleviate financial burdens. Fortunately, there are various government aids that can be utilized to supplement assisted living funds. The most common government aids that can help older adults and families are Medicare and Medicaid.
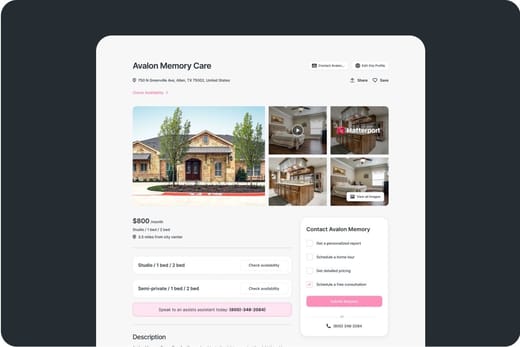
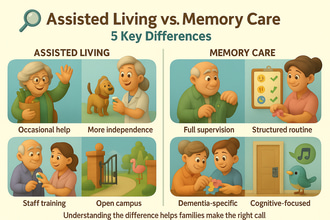
Older adults, especially those needing assistance with activities of daily living (ADLs), like bathing, grooming, and dressing, can benefit from assisted living services. Additionally, assisted living communities also promote social interactions to ensure older adults will not feel lonely. However, older adults and families may hesitate to transition to assisted living due to expenses, so financial aid may help ease financial challenges.
Medicare
One of the most commonly used financial aids for older adults, especially those 65 and older, is Medicare, a federal program that focuses on medical care. Medicare does not cover room and board and focuses on medical services, including prescription drugs and skilled nursing services.
Essentially, Medicare cannot pay for assisted living, but it can cover medical expenses in an assisted living community.
Medicare Part A or Part B can cover necessary long-term care costs intermittently, including
- Intermittent skilled nursing care
- Therapy services, such as physical therapy, occupational therapy, or speech therapy.
- Medical social care services for social and psychological issues.
- Medical supplies and equipment.
Medicare also pays for memory care, which can be helpful for those with cognitive conditions, like Alzheimer’s, Parkinson’s, and Multiple Sclerosis. Additionally, hospice care is also fully covered by Medicare Part A.
Medicaid
Another government aid that can supplement funds for assisted living is Medicaid. It is a federal and state program that helps low-income older adults and people with disabilities. Medicaid also offers Home and Community-Based Services (HCBS) waivers, whose coverage varies by state.
Medicaid typically does not cover board and room, but can cover assisted living services, including:
- Assistance with ADLs, including grooming, dressing, and continence management.
- Transportation
- Housekeeping services
- Recreational activities
- Emergency response systems.
Depending on the state, HCBS waivers of 1915(c) Medicaid waivers can also help with assisted living services.
Eligibility
Focusing on low-income older adults and individuals with disabilities, Medicaid has certain financial and functional requirements that need to be met for eligibility.
Older adults must be 55+ or 65+ to be eligible for Medicaid, and should meet the following:
- Individuals must have an income of at most $1,800 per month, while couples should be earning at most $2,433 per month.
- Asset limits are generally $2,000. However, some states, like California, have already abolished asset limits.
- Assessment by healthcare professionals is also needed to prove the need for financial aid, in terms of medical needs and functionality.
Things to Consider
Since Medicare and Medicaid do not cover room and board, it is better to find supplementary funds, whether personal or state supplementary, like Optional State Supplementation (OSS). Aside from supplementary financial aid, older adults and families should also consider:
- State Variability
- With a wide variation across states, older adults and families can reach out to local agencies for better information.
- Dual eligibilities
- To optimize the benefits of those with both financial aids, older adults should ensure that eligible services are charged to Medicare before Medicaid.
- Older adults should ensure that their chosen assisted living community is Medicare and Medicaid certified.
- HCBS waivers have limited enrollment, so eligibility does not mean immediate enrollment. Hence, other eligible applicants might be subjected to waitlists, resulting in delays in receiving benefits.
Assisted living is a retirement option that helps older adults live comfortably in retirement, helping them with activities of daily living and providing room and board. However, funding assisted living might pose a challenge for those on a budget. Hence, financial aid can help supplement funds. While Medicare does not cover room and board, it can help offset expenses for medical services. Moreover, Medicaid waivers, though varying by state, may also provide help with some assisted living services. To avoid hassles and ensure benefits, it is highly suggested for older adults and families to plan accordingly and enroll as early as they can.