Dementia is a cognitive condition that affects memory, thinking, behavior, and daily functioning. It is a progressive condition that includes Alzheimer’s, vascular dementia, Lewy body dementia, and more. Additionally, the Alzheimer’s Association notes that Alzheimer’s disease affects over 7.2 million Americans 65+, making it the most common form of dementia. Based on the Global Deterioration Scale (GDS) by Dr. Barry Reisberg, the seven-stage model aims to discuss the progression of dementia. With supplementary data from trusted sources like the Alzheimer’s Association, National Institute on Aging (NIA), Cleveland Clinic, and Medical News Today, this article aims to provide comprehensive information about the care needs of each stage.
The 7 Stages
The seven stages are grouped into three general phases: pre-dementia from stages one to three, mild to moderate dementia for stages four to five, and severe dementia, as the final stage from stages six to seven. According to Healthline, the type of dementia and health factors affect the progression of dementia, taking 4 to 20 years from diagnosis to the final stage.
Stage 1: No Cognitive Decline
There are no noticeable symptoms or cognitive impairment. The memory and judgment remain intact, and the individual can still function normally.
- Symptoms
- No behavioral changes or memory lapses.
- ADLs like bathing, dressing, and eating are performed independently.
- The Alzheimer’s Association notes that individuals perform normally on cognitive tests.
- Duration
- This is a baseline state that is indefinite, as noted by Medical News Today.
- Care Needs
- Routine health monitoring would suffice.
- NIA suggests practicing brain-healthy habits.
- Prevalence
- Applies to healthy older adults without dementia pathology, however, undetected brain changes like amyloid plaques may occur, as noted by the Cleveland Clinic.
Stage 2: Very Mild Cognitive Decline
Age-related, minor memory lapses that do not heavily affect daily life. Usually likened to normal aging or stress, however, still not diagnosed as dementia.
- Symptoms
- Misplacing items and forgetting names.
- Minor difficulty with complicated tasks like planning events.
- Healthlines notes that this stage does not affect work and social life.
- Duration
- It may take years, but it may also not progress to dementia without underlying pathology, as noted by NIA.
- Care Needs
- No formal care needed yet; however, monitoring is highly suggested to observe symptoms.
- Medical News Today recommends undergoing cognitive assessments like the Mini-Mental State Exam if necessary.
- Practice mental stimulation and social engagement, and make it a lifestyle.
- Prevalence
- 10 to 15% of older adults 65+ may develop mild cognitive impairment, according to the Cleveland Clinic.
Stage 3 Mild Cognitive Impairment (MCI)
A noticeable decline in cognition beyond normal aging, usually a precursor to dementia. According to NIA, about 30 to 50% of MCI cases progress to dementia within five years.
- Symptoms
- Frequent memory lapses, like forgetting appointments and recent events.
- Difficulty concentrating and finding words.
- Challenges with planning, organizing, or managing finances.
- Healthline also notes a higher level of anxiety and frustration.
- Complex daily tasks become more difficult to perform.
- Duration
- Depending on the progression to dementia, it may take two to seven years.
- Care Needs
- Medical Evaluation to identify the causes of memory lapses, it might be Alzheimer’s or a vitamin deficiency.
- Assistance with complex tasks like paying the bills and medication reminders.
- Family education to prepare for possible progression.
- The Alzheimer’s Association suggests lifestyle changes or cognitive therapies to slow decline.
- Prevalence
- According to the Cleveland Clinic, MCI affects 15 to 20% of older adults 65+.
Stage 4: Mild Dementia
Moderate cognitive decline that affects daily life. According to NIA, Alzheimer’s and other dementias are often confirmed in this stage.
- Symptoms
- Significant memory loss, including forgetting personal history and recent events.
- Difficulty with familiar tasks like cooking, planning, and problem-solving.
- Apathy, mood swings, and social withdrawal.
- Impaired judgment.
- Needs help with some instrumental ADLs like shopping and driving.
- Duration
- According to Medical News Today, this stage may take one to three years before progressing.
- Care Needs
- Formal diagnosis and treatment, including cholinesterase inhibitors for Alzheimer’s.
- Assisted living support for ADLs and complex tasks.
- Home modifications and other safety measures.
- Prevalence
- Known as early dementia. Notably, 1 in 9 older adults 65+ have Alzheimer’s, per Alzheimer’s Association.
Stage 5: Moderate Dementia
According to NIA, individuals may have less autonomy due to significant cognitive decline. Basic ADLs can still be performed.
- Symptoms
- Significant memory gaps, including forgetting current address and names of loved ones.
- Confusion about time, place, and events.
- Difficulty managing hygiene without cues.
- Tendency to wander.
- Increase in agitation and paranoia, causing personality changes.
- Duration
- 1 to 5 years.
- Care Needs
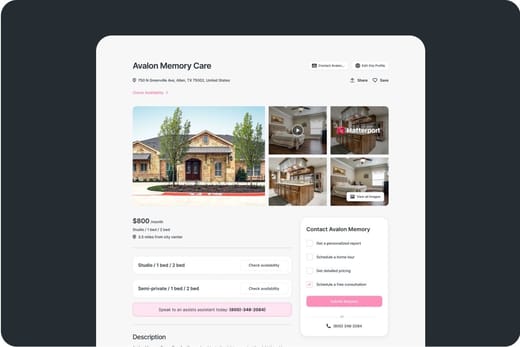
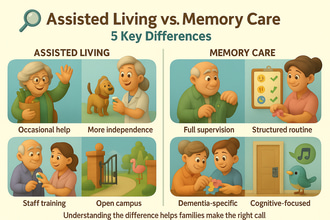
- Memory care in an assisted living facility might be necessary; memory care costs around $7,908 per month.
- Create structured routines and participate in cognitive activities to reduce agitation.
- Implement safety features at home, like alarms.
- Prevalence
- Requires formal care and is most common in those diagnosed with dementia.
Stage 6: Moderately Severe Dementia
Severe cognitive decline, assistance with most ADLs is required. Personality and behavior changes often occur in this stage, per NIA.
- Symptoms
- Loss of awareness of surroundings and recent experiences.
- Inability to recognize loved ones.
- Requires help with basic ADLs, like eating and bathing.
- Increased behavioral issues, including aggression and delusions.
- The Alzheimer’s Association notes that older adults in this stage have a high rish of wandering and may experience sleep disturbances.
- Duration
- 1 to 3 years
- Care Needs
- In need of round-the-clock supervision, a memory care community, which costs $7,908 to $12,000 per month or a nursing home ($9,197 to $10,326 per month), is highly recommended.
- Behavioral management from a dementia-trained team.
- Palliative care discussions for comfort.
- Support groups for families to cope with emotional challenges.
- Prevalence
- Requires institutional care for most.
Stage 7: Severe Dementia
Final stage of progression with significant cognitive and physical decline.
- Symptoms
- Loss of verbal communication, limited to grunts and moans.
- Inability to walk, sit, or swallow without assistance.
- Higher risk for infections, like pneumonia, which is the most common cause of death in dementia.
- Lack of autonomy and complete reliance on caregivers for all ADLs.
- Lack of awareness of surroundings.
- Duration
- Several months to 2 years.
- Care Needs
- Hospice or palliative care at home or in a memory care community and nursing homes, focusing on comfort.
- Nursing home costs around $9,197 to $10,326 per month, while home health care costs $5,625 per month for part-time care, based on Genworth Financial 2025.
- Pain management, infection prevention, and feeding assistance.
- Emotional support to help families facing end-of-life decisions.
- Prevalence
- End-stage dementia often leads to death within 1 to 2 years.
Key Considerations Across Stages
- Progression Variability – The stages are not linear; some may skip stages, especially those with non-Alzheimer’s dementia, as noted by NIA.
- Diagnosis Timing – Healthline notes that stages four to five are common diagnosis points as symptoms become more prominent.
- Behavioral Challenges – Changes in behavior are most common in stages five to six, especially agitation, wandering, and sundowning.
- Family Impact – According to the Alzheimer’s Association, 59% of caregivers are reported to have high stress by stage 5.
Care and Support Strategies
- Early Stages (1 to 3)
- Regular cognitive assessments to detect MCI.
- Implement changes in lifestyle, including 30 minutes of exercise a day, social activities, and cognition-related activities.
- Plan legal and financial matters.
- Requires minimal in-home support or independent living, which costs $3,145 per month.
- Middle Stages (4 to 5)
- Memory care or in-home care ($37 per hour) for safety.
- Assisted living communities are also suggested, which cost $5,676 per month.
- Cognitive therapies, like art and music, can help maintain function.
- Secure residences to prevent wandering.
- Late Stages (6 to 7)
- 24/7 care in specialized environments, like memory care or nursing homes.
- Hospice care to ease pain and discomfort, expenses are often covered by Medicare.
- Grief support and counseling for family members, as recommended by the Alzheimer’s Association.
Funding Care Across Stages
- Medicare
- Covers skilled nursing for up to 100 days and hospice. However, it does not cover long-term memory care and assisted living.
- Medicaid
- Eligible seniors with assets less than $2,000 can receive coverage for memory care and nursing homes.
- Veterans Benefits
- Aid and Attendance provides up to $2,300 per month for eligible Veterans.
- Long-Term Care Insurance
- Covers care costs, especially if purchased early.
- Personal Savings
- Home sales or Social Security can bridge gaps in expenses.
Conclusion
Dementia is a progressive condition, often categorized into seven stages: no impairment to severe decline. These stages discuss the impact of dementia in terms of cognitive, behavioral, and physical abilities. Early stages often show minimal to no decline in cognition, which does not require formal care; however, middle to late stages show significant decline in functionality, hence, formal care is recommended. Understanding the progression of dementia may help families and older adults plan care and manage symptoms. Moreover, early diagnosis will be beneficial in creating tailored plans for care.